Relationship of sodium index with the obesity indicators of university students in Daegu, South Korea: a cross-sectional study
Article information
Abstract
Objectives
The sodium index is an index that converts the estimated sodium intake calculated using a verified and reliable sodium estimation formula. This study aimed to determine the relationship between the sodium index and obesity indicators and the potential impact of excessive sodium consumption on obesity.
Methods
Obesity indicators, such as body mass index (BMI), body fat percentage, waist-to-hip ratio (WHR), and visceral fat levels, were analyzed in 120 university students (60 men and 60 women). The sodium index was calculated by indexing the estimated sodium intake according to age, sex, BMI, salt-eating habits, and salt-eating behaviors. The relationship between sodium index and obesity indicators was analyzed using multiple logistic regression.
Results
The estimated sodium intake was 3,907.1 mg, with 76.7% of the participants categorized under the “careful” level of sodium index and 10.8% under the “moderate” level. As the sodium index increased, the BMI, body fat percentage, WHR, and visceral fat levels significantly increased. All obesity indicators significantly increased in patients with a “severe” sodium index than in those with a “moderate” sodium index. In addition, a strong positive correlation was identified between obesity indicators and sodium index. When the “severe” sodium index was compared with the “moderate” sodium index, the risk of obesity based on body fat percentage increased by 2.181 times (95% confidence interval [CI], 1.526–3.118), while the risk of obesity based on visceral fat level increased by 4.073 times (95% CI, 2.097–7.911).
Conclusions
Our findings suggest a correlation between excessive sodium intake and obesity. Moreover, the sodium index can be used to determine sodium intake.
INTRODUCTION
According to the World Health Organization, 43% of adults worldwide were overweight and 16% were obese in 2022 [1]. Obesity is associated with numerous health conditions such as hypertension, cardiovascular disease, stroke, diabetes, metabolic syndrome, cancer, and respiratory disorders [2-5]. A 5 kg increase in weight corresponds to an approximately 5% increased risk of developing colon cancer [6], while a higher the body mass index (BMI) increases the likelihood of developing type 2 diabetes [7]. The prevalence of obesity in South Korea increased from 31.8% (37.7% in men and 25.1% in women) in 2013 to 37.2% (47.7% in men and 25.7% in women) in 2022 [8]. Abdominal obesity, determined by waist circumference, increased by 12% to 39.4% in 2019 compared with that in 2007 [9].
Abdominal obesity is associated with the development of cardiovascular disease and diabetes; even in individuals with a BMI of 25 kg/m2, a high waist circumference (> 102 cm in men and > 88 cm in women) correlates with an increased risk of cardiovascular disease and diabetes [10]. Among Asians, those with a BMI of ≥ 25 kg/m2 had a higher incidence of type 2 diabetes and cardiovascular disease [11]. According to a 2020 report from Mexico, body fat mass was more strongly associated with type 2 diabetes than BMI [12].
The daily average sodium intake of Koreans decreased from 4,789.2 mg in 2010 to 3,030.2 mg in 2022. However, it is still more than twice the recommended intake level [8,13]. Excessive sodium intake has been shown to increase the risk of diseases, such as hypertension, stroke, cardiovascular disease, and gastric cancer [14-17].
Excessive sodium intake has been consistently linked to an increased risk of obesity in both domestic and international studies. Higher sodium intake was associated with higher BMI, waist circumference, abdominal computed tomography, and visceral fat mass [18-20]. A study conducted in the United Kingdom revealed that the group with a higher 24-hour urinary sodium excretion had an increased risk of obesity compared with the group with a lower excretion [21]. In a study conducted on Spanish adults, the group with a higher 24-hour urinary sodium excretion had a higher BMI than the group with a lower excretion [22]. According to the National Health and Nutrition Examination Survey conducted in the United States, sodium intake is independently correlated with being overweight and obesity [23]. Moreover, an analysis using data from the Korea National Health and Nutrition Examination Survey on sodium density and obesity revealed that sodium intake was a risk factor for obesity, regardless of calorie intake [24]. Additionally, Nam et al. [25] showed that individuals in the highest quartile of 24-hour urinary sodium concentration had a higher risk of obesity compared with the remaining participants.
Although previous studies have examined the relationship between sodium intake, 24-hour urinary sodium excretion, and obesity, no study has analyzed the association between the sodium index and obesity indicators. The sodium index is derived from the estimated sodium intake, calculated using a validated and reliable regression equation, and it was developed by analyzing the 24-hour dietary intake and 24-hour urinary sodium excretion data from various population groups across 4 regions of South Korea [26].
This study aimed to investigate the sodium index in university students and measure the obesity-related indicators to analyze the correlation between sodium intake and obesity. We aimed to evaluate the potential utility of sodium index as a tool for assessing sodium intake.
METHODS
Ethics statement
Obtainment of informed consent was exempted by the Institutional Review Board (IRB) of Kyungpook National University (approval number: IRB No. 2018-O146)
1. Study subjects
The study included university students residing in the Daegu area recruited through the university website and social networking service channels. A total of 120 participants (60 men and 60 women) were enrolled. A sodium index survey was conducted using an online questionnaire from October 1 to 31, 2018. Body composition measurements, including body fat analysis, were performed during onsite visits from October 23 to 31, 2018.
2. Anthropometrics
Body measurements were performed on the study participants using a body composition analyzer (Inbody XBIA 900; JW, Soeul, Korea) to assess weight, BMI, body fat percentage, waist-to-hip ratio (WHR), and visceral fat level. BMI was classified as follows according to the Korean Society for the Study of Obesity and the World Health Organization Asia-Pacific Region Obesity guidelines [27]: < 18.5 as underweight, 18.5–22.9 as normal, 23–24.9 as overweight, and ≥ 25 as obesity. Additionally, obesity based on body fat percentage was classified based on the modified version of the criteria used in Lee and Nieman’s study [28] and established by the Korean Society for Health Promotion and Disease Prevention [29]. In men, body fat percentages of < 8% indicate underweight; 8%–15%, moderate; > 15% and < 25%, overfat; and ≥ 25%, obesity. In women, body fat percentages of < 15% indicate underweight; 15%–25%, moderate; > 25% and < 30%, overfat; and ≥ 30%, obesity.
3. Sodium index survey
The sodium index was calculated using the method described by Lee et al. [26]. The participants’ sex, age, BMI, salt-eating habits, and dietary behaviors were surveyed, and sodium intake was estimated using a regression equation, which was then converted into the sodium index.
To assess salty-eating habits, the participants were asked about their tendency to consume salty foods, and their responses were rated as follows: “eat unsalty,” 10 points; “eat slightly unsalty,” 20 points; “eat neither unsalty nor salty,” 30 points; “eat slightly salty,” 40 points; and “eat salty,” 50 points.
A questionnaire was used to evaluate salty dietary behavior, which comprised 3 items regarding salty-eating behavior, 2 items regarding sodium reduction behavior, 3 items regarding the frequency of salty food intake, and 2 items regarding the frequency of low-sodium food intake. The participants’ dietary behavior was rated as follows: “not at all,” 2 points; “slightly,” 4 points; “moderately,” 6 points; “very,” 8 points; and “extremely,” 10 points. Meanwhile, the food intake frequency scores were as follows: 3 times a month, 2 points; 1–2 times a week, 4 points; 3–6 times a week, 6 points; once a day, 8 points; and 2–3 times a day, 10 points. Conversely, the scoring system for sodium reduction behaviors and low-sodium food intake frequencies was reversed.
Sodium Intake Estimation Regression Equation = −191.9 + (−705.2 × Sex1)) + (189.6 × G_age2)) + (130.6 × BMI) + (24.2 × Eating Habit3)) + (18.5 × Dietary Behavior4))
1)1 = men, 2 = women; 2)1 = 19–29, 2 = 30–39, 3 = 40–49, 4 = 50–59, 5 = 60–69;
3)10 = unsalty, 20 = slightly unsalty, 30 = neither unsalty nor salty, 40 = slightly salty, 50 = salty;
4)20–100 of a total of 10 items.
The criteria used for evaluating the sodium index were as follows:
The estimated sodium intake of 1,500 to < 2,000 mg: 75 to < 100 points was rated as “very moderate,” 2,000 to < 3,000 mg: 100 to < 150 points as “moderate,” < 1,500 mg or 3,000 to < 5,000 mg: < 75 points or 150 to < 250 points as “careful,” and ≥ 5,000 mg: ≥ 250 points as “severe.”
4. Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics 27 (IBM Corporation, Armonk, NY, USA). The significant differences in obesity indicators, estimated sodium intake, and sodium index according to sex were assessed using t-tests and χ2 analyses. One-way analysis of variance was used to compare the obesity indicators across quartiles of the sodium index and to assess the sodium index across levels of obesity indicators, followed by Duncan’s multiple range test for post-hoc analysis. The significance level for all items was set at a P-value of < 0.05. The correlation between obesity indicators and the sodium index was analyzed using Pearson’s correlation analysis. Multiple logistic regression analysis was conducted, adjusting for age and sex, to examine the relationship between sodium index and obesity indicators.
RESULTS
1. Obesity indicators and sodium index
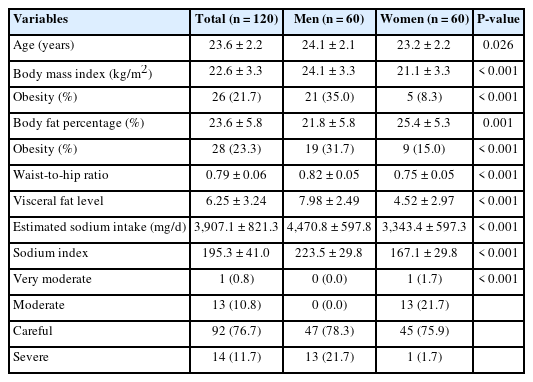
Table 1 discusses the participants’ body measurements and sodium indices. The mean BMI was 22.6 kg/m2 (obesity rate: 21.7%), the mean body fat percentage was 23.6% (obesity rate: 23.3%), the mean WHR was 0.79, and the mean visceral fat level was 6.25. Body fat percentage was higher in female students than in male students (P < 0.001), while the BMI, WHR, and visceral fat levels were higher in male students than in female students (all P < 0.001).
The estimated mean sodium intake was 3,907.1 mg, with male students (4,470.8 mg) having a higher intake than female students (3,343.4 mg) (P < 0.001). Similarly, the mean sodium index was 195.3, which was higher in male students (223.5) than in female students (167.1) (P < 0.001). The distribution of sodium index showed that 76.7% of the total participants were at the “careful” level. Among male students, none showed a “moderate” level, 78.3% demonstrated a “careful” level, and 21.7% reached a “severe” level. These results were higher than the percentages observed among female students (“careful”: 75.9%, “severe”: 1.7%; P < 0.001).
2. Salty-eating habits and dietary behaviors
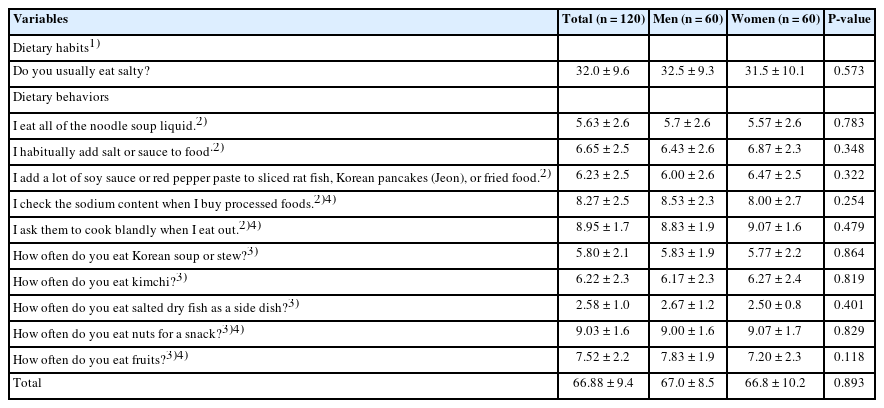
Table 2 discusses the survey results related to the salt-eating habits and dietary behaviors of the study participants. Among the salty-eating behavior items (total score: 10), the item “How often do you eat salted dry fish as a side dish?” obtained the lowest score (2.58), indicating the infrequent consumption of salted fish among university students. Additionally, the item “I check the sodium content when I buy processed foods” obtained a score of 8.27, suggesting that a high proportion of students did not check the sodium content. Conversely, the items “I ask them to cook blandly when I eat out” (8.95) and “How often do you eat nuts for a snack?” (9.03) obtained higher scores, implying rare requests for less salty options when dining out and the infrequent consumption of nuts as snacks. No significant differences were observed in the eating habits or dietary behaviors between male and female students.
3. Comparison of obesity indicators by quartiles of sodium index
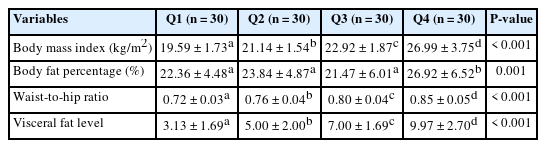
Table 3 lists a comparison of obesity indicators according to the quartiles of sodium. BMI, WHR, and visceral fat level showed significant differences across all quartiles (from Q1 to Q4). This finding suggests that BMI, WHR, and visceral fat levels increased as the sodium index increased (P < 0.05). With regard to body fat percentage, Q4 (26.92%) was significantly higher than Q1–Q3 (P < 0.05).
4. Comparison of obesity indicators by sodium index level
Figure 1 depicts a comparison of obesity indicators according to sodium index level. The group with a “moderate” sodium index level demonstrated significantly lower BMI, WHR, and visceral fat levels compared with the group that reached “careful” and “severe” levels (P < 0.05). Body fat percentage was significantly higher in the “severe” group than in the “moderate” and “careful” groups (P < 0.05).
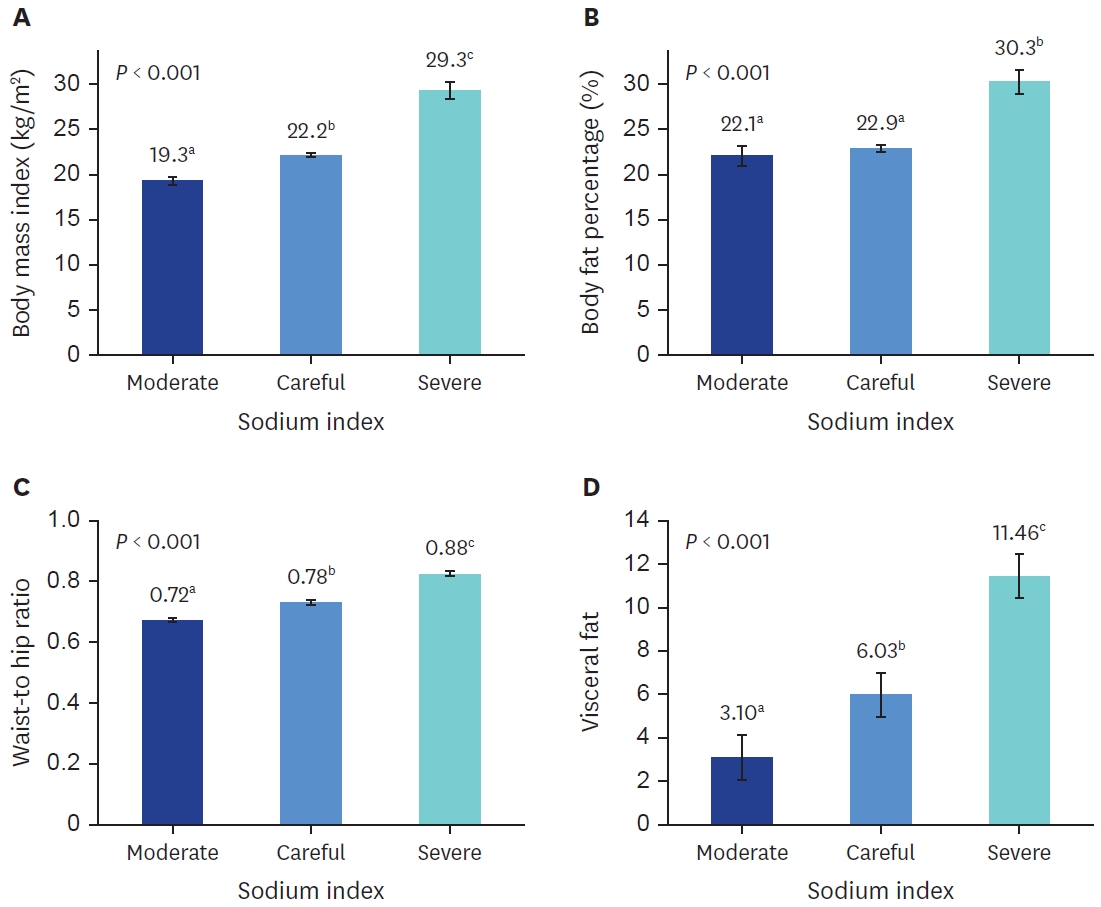
Comparison of obesity index according to sodium index. (A) Body mass index; (B) Body fat percentage; (C) Waist-to-hip ratio; (D) Visceral fat. Bars indicate the mean ± standard error. Means with different lower case letters in the same column are significantly different by Duncan’s multiple range test with a P-value of < 0.05.
5. Comparison of sodium index by obesity indicators
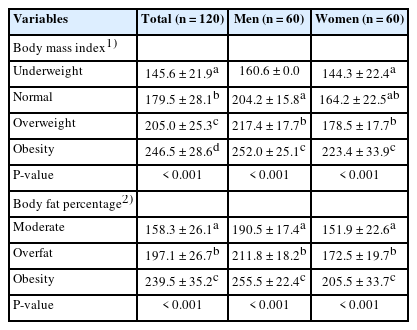
Table 4 discusses the results of the comparison of sodium index according to the degree of obesity based on BMI and body fat percentage. Based on the BMI classification, the mean sodium index for underweight participants was 145.6, which significantly increased to 179.5 for normal-weight participants, 205.0 for overweight participants, and 246.5 for obese participants (P < 0.05). The same trend was observed in both male and female students.
Based on the body fat percentage classification, the sodium index for the moderate category was 158.3, which was significantly lower than 197.1 for the overfat category and 239.5 for the obesity category (P < 0.05). Similarly, this trend was observed in both male and female students.
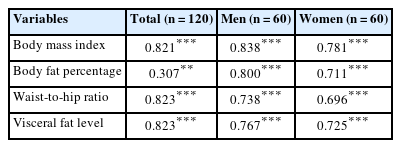
6. Correlation between sodium index and obesity indicators
Table 5 discusses the results of the correlation analysis between sodium index and obesity indicators. The sodium index showed a high positive correlation with BMI (P < 0.001), body fat percentage (P < 0.01), WHR (P < 0.001), and visceral fat level (P < 0.001); the same trend was observed for both male and female students.
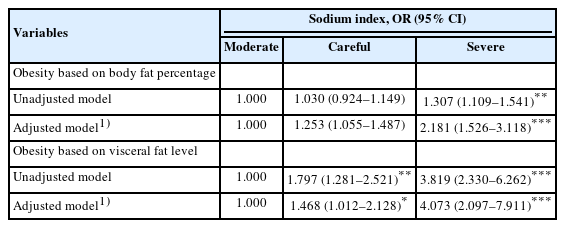
7. Relationship of sodium index with obesity indicators
The results of the analysis of the effect of sodium index on obesity indicators before and after adjusting for confounding variables are represented in Table 6. Using the “moderate” sodium index level corresponding to an estimated sodium intake of 2,000 to < 3,000 mg as a reference, participants who reached the “careful” (3,000 to < 5,000 mg) and “severe” (≥ 5,000 mg) levels had 1.253 times (95% confidence interval [CI], 1.055–1.487) and 2.181 times (95% CI, 1.526–3.118) higher risk of developing obesity based on the body fat percentage, respectively. Additionally, compared with those with a “moderate” sodium index level, participants who reached the “careful” and “severe” levels had 1.468 times (95% CI, 1.012–2.128) and 4.073 times (95% CI, 2.097–7.911) higher risk of developing obesity based on the visceral fat level, respectively.
DISCUSSION
In this study, we investigated the potential impact of excessive sodium intake on obesity among university students by analyzing the relationship between sodium index and obesity indicators (BMI, body fat percentage, WHR, and visceral fat level). A strong correlation was observed between the sodium index and obesity indicators. Compared with individuals with a “moderate” sodium index level, those with a “severe” level had 2-fold and 4-fold higher risks of developing obesity based on the body fat percentage and visceral fat level, respectively. This underscores the association between higher sodium intake and an increased likelihood of obesity.
Epidemiological studies have consistently demonstrated that excessive sodium intake is associated with triglyceride level, blood glucose level, waist circumference, body fat percentage, metabolic syndrome, and insulin resistance [30,31]. Additionally, a previous study that examined the relationship between sodium intake and obesity in adults reported that weight, BMI, and total energy intake significantly increased in both men and women as sodium intake increased [32]. Moreover, an experimental study on the obesity pathogenesis of a high-sodium diet in rats revealed that higher sodium intake increases fat synthesis in the liver and fat accumulation in both the liver and adipose tissue, thereby reducing heat generation and increasing the risk of obesity [33].
In our study, the sodium index developed by analyzing the 24-hour dietary intake and 24-hour urinary sodium excretion showed significant correlations with BMI, body fat percentage, WHR, and visceral fat levels. This observation suggests that higher estimated sodium intake or excessive sodium consumption increases the risk of developing obesity. This result supports the findings of previous studies, which indicated that higher 24-hour urinary sodium excretion is associated with an increased risk of abdominal obesity [20]. When the sodium index was divided into quartiles, individuals in the top 25% of the sodium index had higher obesity indicators than those in the bottom 25%. Given that a higher sodium index corresponds to a greater probability of obesity, it could serve as a tool for assessing sodium intake.
However, this study has certain limitations. The study only evaluated 120 university students from one region, and the distribution of obesity among the participants was not even.
Previous studies have demonstrated the significance of sodium reduction in preventing obesity and diabetes, managing hypertension, cardiovascular diseases, Alzheimer’s disease, and other conditions, thus reducing healthcare costs [34,35]. Therefore, to establish low-salt eating habits and prevent obesity, metabolic syndrome, hypertension, cardiovascular diseases, and other chronic diseases, the sodium index should be utilized. As excessive sodium intake affects the development of obesity and chronic diseases, promoting low-salt eating habits for obesity prevention and management is essential. This approach can improve individual quality of life and reduce social costs and medical expenses associated with obesity.
CONCLUSIONS
A study conducted among 120 university students in Daegu, South Korea reported a high correlation between the sodium index and obesity indicators (BMI, body fat percentage, WHR, and visceral fat level). Specifically, as the sodium index increased, all obesity indicators increased significantly. At the “severe” sodium index level, the risk of obesity determined by body fat percentage was 2.181 times higher, and the risk of obesity determined by visceral fat level was 4.073 times higher compared with that at the “moderate” level. These results confirm that excessive sodium intake increases the risk of obesity and suggest that the sodium index could serve as a useful tool for assessing sodium intake levels in individuals.
Notes
Conflict of Interest
There are no financial or other issues that might lead to conflict of interest.
Data Availability
The participants of this study did not give written consent for their data to be shared publicly, so due to the sensitive nature of the research supporting data is not available.