Articles
- Page Path
- HOME > Korean J Community Nutr > Volume 20(6); 2015 > Article
-
Research Article
- Associations between 24-hour Urine Sodium Excretion Level and Obesity-related Metabolic Risk Factors
- Hyun Woo Oh, Hyun Jung Kim, Dae Won Jun, Seung Min Lee
-
Korean Journal of Community Nutrition 2015;20(6):460-467.
DOI: https://doi.org/10.5720/kjcn.2015.20.6.460
Published online: December 31, 2015
1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
2Department of Food and Nutrition, Sungshin Women's University, Seoul, Korea.
- Corresponding author: Seung Min Lee. Department of Food and Nutrition, Sungshin Women's University, 55, Dobong-ro76gagil, Gangbuk-gu, Seoul 01133, Korea. Tel: (02) 920-7671, Fax: (02) 920-2076, smlee@sungshin.ac.kr
Copyright © 2015 The Korean Society of Community Nutrition
This is an Open-Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 152 Views
- 1 Download
- 7 Crossref
Abstract
-
Objectives
- Excess sodium intake has been linked to obesity and obesity-related indices. However, the scientific evidence for this association is inadequate. The purpose of this study was to investigate the association between urinary sodium excretion and obesity-related indices among Korean adults.
-
Methods
- A convenience sample of 120 subjects (60 obese and 60 non-obese subjects) were recruited applying frequency matching for sex and age between two groups. Sodium intake level was assessed through 24-hour urine collection. Obesity-related metabolic risk factors, including fasting blood lipid indices, subcutaneous and visceral fat through computed tomography (CT), insulin resistance indices, blood pressure and liver enzymes were measured in all subjects. These obesity-related metabolic risk factors were compared between obese and non-obese group according to sodium excretion levels (<110 mEq/day, 110~180 mEq/day, >180 mEq/day).
-
Results
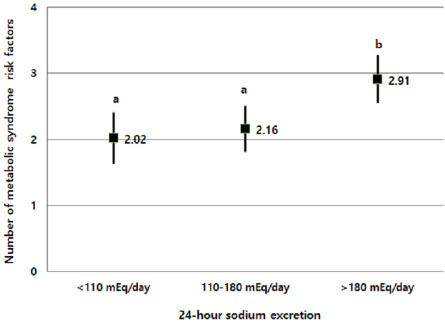
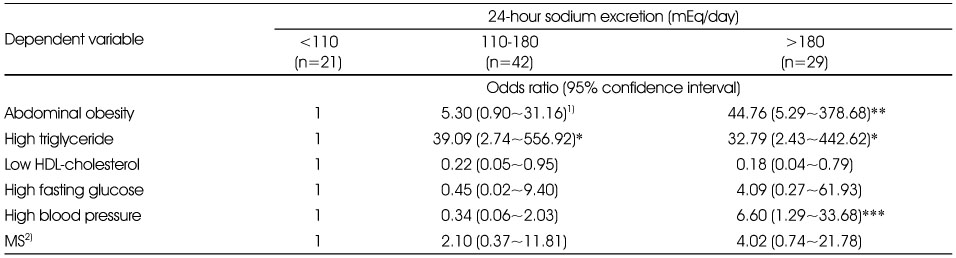
- After adjusting for age, gender, health behaviors (smoking, exercise, drinking), and energy intake, several obesity-related metabolic risk factors, including abdominal circumference, body fat percentage, subcutaneous and visceral fat, triglyceride, and systolic blood pressure were found to be significantly deteriorated as the sodium excretion level increases. In addition, multivariate adjusted-odds ratios of abdominal obesity, high blood triglyceride, and high blood pressure were found significantly higher in the highest sodium excretion group compared to the lowest group. The mean number of metabolic syndrome risk factors was also significantly greater in the highest sodium excretion group than in the lowest group.
-
Conclusions
- The current study findings suggested that high sodium intake can affect obesity and metabolic syndrome risk negatively, implying the necessity of future research on low-sodium diet intervention in relation to obesity and related health problems.
- 1. Ministry of Health and Welfare & Korea Centers for Disease Control and Prevention. Korea Health Statistics 2013: Korea National Health and Nutrition Examination Survey (KNHANES VI-1) [internet]. 2014; cited 2015 Aug 10]. Available from: https://knhanes.cdc.go.kr/.
- 2. Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010; 362(7): 590-599.ArticlePubMedPMC
- 3. Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet 2007; 370(9604): 2044-2053.ArticlePubMed
- 4. Song HJ, Cho YG, Lee HJ. Dietary sodium intake and prevalence of overweight in adults. Metabolism 2013; 62(5): 703-708.ArticlePubMed
- 5. Yoon YS, Oh SW. Sodium density and obesity; the Korea National Health and Nutrition Examination Survey 2007-2010. Eur J Clin Nutr 2013; 67(2): 141-146.ArticlePubMedPDF
- 6. He FJ, Marrero NM, MacGregor GA. Salt intake is related to soft drink consumption in children and adolescents: a link to obesity? Hypertension 2008; 51(3): 629-634.ArticlePubMed
- 7. Hoffmann IS, Cubeddu LX. Salt and the metabolic syndrome. Nutr Metab Cardiovasc Dis 2009; 19(2): 123-128.ArticlePubMed
- 8. Larsen SC, Ängquist L, Sørensen TI, Heitmann BL. 24h urinary sodium excretion and subsequent change in weight, waist circumference and body composition. PLoS One 2013; 8(7): e69689.ArticlePubMedPMC
- 9. Räisänen JP, Silaste ML, Kesäniemi YA, Ukkola O. Increased daily sodium intake is an independent dietary indicator of the metabolic syndrome in middle-aged subjects. Ann Med 2012; 44(6): 627-634.ArticlePubMed
- 10. Moon HK, Kong JE. Assessment of nutrient intake for middle aged with and without metabolic syndrome using 2005 and 2007 Korean National Health and Nutrition Survey. Korean J Nutr 2010; 43(1): 69-78.Article
- 11. Yoo HJ, Kim YH. A study on the characteristics of nutrient intake in metabolic syndrome subjects. Korean J Nutr 2008; 41(6): 510-517.
- 12. Hu G, Jousilahti P, Peltonen M, Lindstrom J, Tuomilehto J. Urinary sodium and potassium excretion and the risk of type 2 diabetes: a prospective study in Finland. Diabetologia 2005; 48(8): 1477-1483.ArticlePubMedPDF
- 13. Hong AR, Lim S. Clinical characteristics of metabolic syndrome in Korea, and its comparison with other Asian countries. J Diabetes Investig 2015; 6(5): 508-515.PubMedPMC
- 14. Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ 1988; 297: 319-327.ArticlePubMedPMC
- 15. Ji C, Sykes L, Paul C, Dary O, Legetic B, Campbell NR, et al. Sub-group for research and surveillance of the PAHO-WHO regional expert group for cardiovascular disease prevention through population-wide dietary salt reduction. Systematic review of studies comparing 24-hour and spot urine collections for estimating population salt intake. Rev Panam Salud Publica 2012; 32(4): 307-315.ArticlePubMed
- 16. Kissebah AH, Vydelingum N, Murray R, Evans DJ, Kalkhoff RK, Adams PW. Relation of body fat distribution to metabolic complications of obesity. J Clin Endocrinol Metab 1982; 54(2): 254-260.ArticlePubMed
- 17. Park HS, Lim SY. Visceral fat accumulation according to sex & age, and in relation to cardiovascular risk factors in Korean obese men & women. Korean J Obes 1998; 7(4): 342-354.
- 18. Fujioka S, Matsuzawa Y, Tokunaga K, Tarui S. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism 1987; 36(1): 54-59.ArticlePubMed
- 19. Chen J, Gu D, Huang J, Rao DC, Jaquish CE, Hixson JE, et al. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: a dietary intervention study. Lancet 2009; 373(9666): 829-835.ArticlePubMedPMC
- 20. Rhee MY, Kim JH, Kim YS, Chung JW, Bae JH, Nah DY, et al. High sodium intake in women with metabolic syndrome. Korean Circ J 2014; 44(1): 30-36.ArticlePubMedPMC
- 21. Perry CG, Palmer T, Cleland SJ, Morton IJ, Salt IP, Petrie JR, et al. Decreased insulin sensitivity during dietary sodium restriction is not mediated by effects of angiotensin II on insulin action. Clin Sci (Lond) 2003; 105(2): 187-194.ArticlePubMedPDF
- 22. Townsend RR, Kapoor S, McFadden CB. Salt intake and insulin sensitivity in healthy human volunteers. Clin Sci (Lond) 2007; 113(3): 141-148.ArticlePubMedPDF
- 23. Fliser D, Fode P, Arnold U, Nowicki M, Kohl B, Ritz E. The effect of dietary salt on insulin sensitivity. Eur J Clin Invest 1995; 25(1): 39-43.Article
- 24. Foo M, Denver AE, Coppack SW, Yudkin JS. Effect of salt-loading on blood pressure, insulin sensitivity and limb blood flow in normal subjects. Clin Sci (Lond) 1998; 95(2): 157-164.ArticlePDF
- 25. Donovan DS, Solomon CG, Seely EW, Williams GH, Simonson DC. Effect of sodium intake on insulin sensitivity. Am J Physiol 1993; 264(5): E730-E734.Article
- 26. Gruska S, Wolf E, Jendral I, Wedler B, Kraatz G. Salt sensitivity and insulin resistance in normotensives. Exp Clin Endocrinol Diabetes 1997; 105: Suppl 2. 22-26.Article
- 27. Gomi T, Shibuya Y, Sakurai J, Hirawa N, Hasegawa K, Ikeda T. Strict dietary sodium reduction worsens insulin sensitivity by increasing sympathetic nervous activity in patients with primary hypertension. Am J Hypertens 1998; 11(9): 1048-1055.ArticlePubMed
- 28. Petrie JR, Morris AD, Minamisawa K, Hilditch TE, Elliott HL, Small M, et al. Dietary sodium restriction impairs insulin sensitivity in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 1998; 83(5): 1552-1557.ArticlePubMed
- 29. Sharma AM, Ruland K, Spies KP, Distler A. Salt sensitivity in young normotensive subjects is associated with a hyperinsulinemic response to oral glucose. J Hypertens 1991; 9(4): 329-335.ArticlePubMed
- 30. Iwaoka T, Umeda T, Inoue J, Naomi S, Sasaki M, Fujimoto Y, et al. Dietary NaCl restriction deteriorates oral glucose tolerance in hypertensive patients with impairment of glucose tolerance. Am J Hypertens 1994; 7(5): 460-463.ArticlePubMed
- 31. Iwaoka T, Umeda T, Ohno M, Inoue J, Naomi S, Sato T, et al. The effect of low and high NaCl diets on oral glucose tolerance. Klin Wochenschr 1988; 66(16): 724-728.ArticlePubMedPDF
- 32. Inoue J, Cappuccio FP, Sagnella GA, Markandu ND, Folkerd EJ, Sampson B, et al. Glucose load and renal sodium handling in mild essential hypertension on different sodium intakes. J Hum Hypertens 1996; 10(8): 523-529.
- 33. Ames RP. The effect of sodium supplementation on glucose tolerance and insulin concentrations in patients with hypertension and diabetes mellitus. Am J Hypertens 2001; 14(7): 653-659.Article
- 34. Meland E, Laerum E, Aakvaag A, Ulvik RJ, Høstmark AT. Salt restriction: effects on lipids and insulin production in hypertensive patients. Scand J Clin Lab Invest 1997; 57(6): 501-505.Article
- 35. Ferri C, Bellini C, Desideri G, Giuliani E, De Siati L, Cicogna S, et al. Clustering of endothelial markers of vascular damage in human salt-sensitive hypertension: influence of dietary sodium load and depletion. Hypertension 1998; 32(5): 862-868.ArticlePubMed
- 36. Grey A, Braatvedt G, Holdaway I. Moderate dietary salt restriction does not alter insulin resistance or serum lipids in normal men. Am J Hypertens 1996; 9(4 Pt 1): 317-322.Article
- 37. Kerstens MN, van der Kleij FG, Boonstra AH, Sluiter WJ, Koerts J, Navis G, et al. Salt loading affects cortisol metabolism in normotensive subjects: relationships with salt sensitivity. J Clin Endocrinol Metab 2003; 88(9): 4180-4185.ArticlePDF
- 38. Lopes HF, Martin KL, Nashar K, Morrow JD, Goodfriend TL, Egan BM. DASH diet lowers blood pressure and lipid-induced oxidative stress in obesity. Hypertension 2003; 41(3): 422-430.Article
- 39. Kuroda S, Uzu T, Fujii T, Nishimura M, Nakamura S, Inenaga T, et al. Role of insulin resistance in the genesis of sodium sensitivity in essential hypertension. J Hum Hypertens 1999; 13(4): 257-262.ArticlePubMedPDF
- 40. Blumenthal JA, Babyak MA, Sherwood A, Craighead L, Lin PH, Johnson J, et al. Effects of the dietary approaches to stop hypertension diet alone and in combination with exercise and caloric restriction on insulin sensitivity and lipids. Hypertension 2010; 55(5): 1199-1205.Article
- 41. Suzuki M, Kimura Y, Tsushima M, Harano Y. Association of insulin resistance with salt sensitivity and nocturnal fall of blood pressure. Hypertension 2000; 35(4): 864-868.ArticlePubMed
- 42. Facchini FS, DoNascimento C, Reaven GM, Yip JW, Ni XP, Humphreys MH. Blood pressure, sodium intake, insulin resistance, and urinary nitrate excretion. Hypertension 1999; 33(4): 1008-1012.ArticlePubMed
- 43. Sharma AM, Schorr U, Distler A. Insulin resistance in young salt-sensitive normotensive subjects. Hypertension 1993; 21(3): 273-279.Article
- 44. Dengel DR, Mayuga RS, Kairis GM, Goldberg AP, Weir MR. Effect of dietary sodium on insulin sensitivity in older, obese, sedentary hypertensives. Am J Hypertens 1997; 10(9 Pt 1): 964-970.ArticlePubMed
- 45. Khaw KT, Bingham S, Welch A, Luben R, O'Brien E, Wareham N, et al. Blood pressure and urinary sodium in men and women: the Norfolk cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk). Am J Clin Nutr 2004; 80(5): 1397-1403.Article
- 46. Karppanen H, Mervaala E. Sodium intake and hypertension. Prog Cardiovasc Dis 2006; 49(2): 59-75.ArticlePubMed
REFERENCES
Mean numbers1) of metabolic syndrome risk factors according to according to 24-hour sodium excretion levels
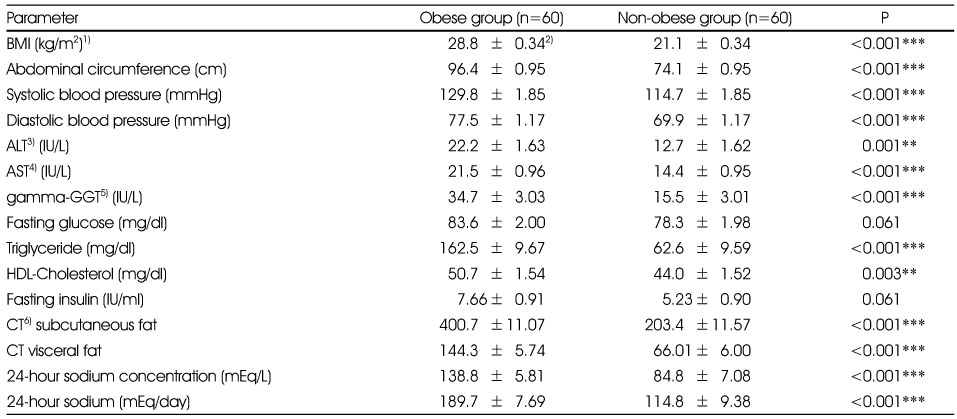
Comparison of obesity and obesity-related metabolic indices between obese and non-obese groups
Comparison of obesity and obesity-related metabolic indices according to 24-hour urine sodium excretion levels
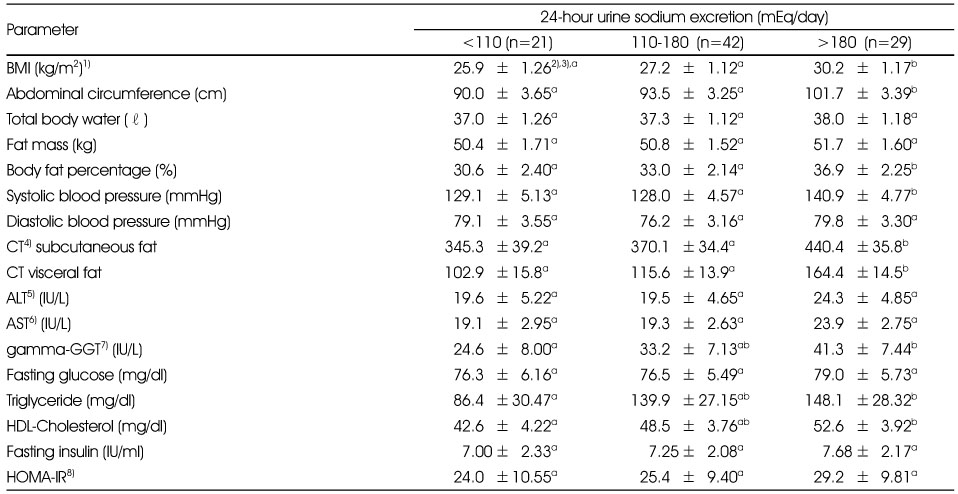
1) BMI: body mass index
2) Mean ±SE
3) Adjusted for age (years), sex, smoking (no smoking, previous smoking. current smoking), drinking (no drinking, 1~4 times/month, >=5 times/month), physical activity (rarely, 1~2 times/week, >=3 times/week), energy intake (kcal/day)
4) CT: computed tomography
5) ALT: alanine transferase
6) AST: aspartate transferase
7) GGT: glutamyl transferase
8) HOMA-IR: homeostasis model assessment of insulin resistance
ab: Different alphabet letters within a row represent significant difference (p < 0.05) by Tukey-Kramer's multiple comparison test.
Spearman correlation coefficient between obesity-related indices and 24-hour urine sodium excretion levels
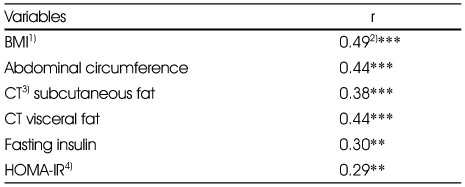
Figure & Data
REFERENCES
Citations

- Relationship of sodium index with the obesity indicators of university students in Daegu, South Korea: a cross-sectional study
Young-Won Jang, Jian Ma, Yeon-Kyung Lee
Korean Journal of Community Nutrition.2024; 29(3): 189. CrossRef - Dietary salt intake and kidney function in rural Senegalese populations: a cross-sectional study
Ndongo Modou, Lot Nehemie Motoula Latou, Toure Maimouna, Amadou Diop Dia, Sidy Mohamed Seck
Journal of Health, Population and Nutrition.2024;[Epub] CrossRef - The association between dietary sodium intake and obesity in adults by sodium intake assessment methods: a review of systematic reviews and re-meta-analysis
Jounghee Lee, Cheongmin Sohn, Oh-Yoen Kim, Young-Min Lee, Mi Ock Yoon, Myoungsook Lee
Nutrition Research and Practice.2023; 17(2): 175. CrossRef - Relationship between urinary sodium-creatinine ratios and insulin resistance in Korean children and adolescents with obesity
So Yoon Han, Nan Hee Kim, Do Hoon Kim, Kyungdo Han, Seon Mee Kim
Journal of Pediatric Endocrinology and Metabolism.2018; 31(4): 375. CrossRef - Association between Sodium Excretion and Obesity of Adults in Gwangju
Mijin Jo, Young-Ran Heo
Korean Journal of Community Nutrition.2018; 23(1): 38. CrossRef - Relationship of sodium consumption with obesity in Korean adults based on Korea National Health and Nutrition Examination Survey 2010~2014
Se Young Cheon, Hye Won Wang, Hwa Jung Lee, Kyung Mi Hwang, Hae Seong Yoon, Yoon Jung Kang
Journal of Nutrition and Health.2017; 50(1): 64. CrossRef - Associations of Obesity and Dyslipidemia with Intake of Sodium, Fat, and Sugar among Koreans: a Qualitative Systematic Review
Yoon Jung Kang, Hye Won Wang, Se Young Cheon, Hwa Jung Lee, Kyung Mi Hwang, Hae Seong Yoon
Clinical Nutrition Research.2016; 5(4): 290. CrossRef
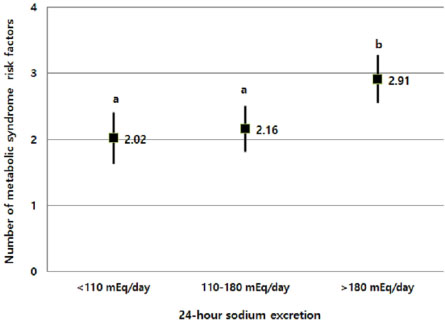
Fig. 1
Comparison of obesity and obesity-related metabolic indices between obese and non-obese groups
1) BMI: body mass index
2) Mean±SE
3) ALT: alanine transferase
4) AST: aspartate transferase
5) GGT: glutamyl transferase
6) CT: computed tomography
**: p < 0.01, ***: p < 0.001
Comparison of obesity and obesity-related metabolic indices according to 24-hour urine sodium excretion levels
1) BMI: body mass index
2) Mean ±SE
3) Adjusted for age (years), sex, smoking (no smoking, previous smoking. current smoking), drinking (no drinking, 1~4 times/month, >=5 times/month), physical activity (rarely, 1~2 times/week, >=3 times/week), energy intake (kcal/day)
4) CT: computed tomography
5) ALT: alanine transferase
6) AST: aspartate transferase
7) GGT: glutamyl transferase
8) HOMA-IR: homeostasis model assessment of insulin resistance
ab: Different alphabet letters within a row represent significant difference (p < 0.05) by Tukey-Kramer's multiple comparison test.
Spearman correlation coefficient between obesity-related indices and 24-hour urine sodium excretion levels
1) BMI: body mass index
2) Adjusted for age (years) and energy intake (kcal/day)
3) CT: computed tomography
4) HOMA-IR: homeostasis model assessment of insulin resistance
**: p < 0.01, ***: p < 0.001 by partial Spearman correlation analysis
Odds radios of metabolic syndrome risk factors and metabolic syndrome according to 24-hour sodium excretion levels
1) Adjusted for age(years), sex, smoking (no smoking, previous smoking. current smoking), drinking(no drinking, 1~4 times/month, >=5 times/month), physical activity(rarely, 1~2 times/week, >=3 times/week), energy intake (kcal/day)
2) MS : Metabolic syndrome
*: p < 0.05, **: p < 0.01, ***: p < 0.001
1) BMI: body mass index 2) Mean±SE 3) ALT: alanine transferase 4) AST: aspartate transferase 5) GGT: glutamyl transferase 6) CT: computed tomography **:
1) BMI: body mass index 2) Mean ±SE 3) Adjusted for age (years), sex, smoking (no smoking, previous smoking. current smoking), drinking (no drinking, 1~4 times/month, >=5 times/month), physical activity (rarely, 1~2 times/week, >=3 times/week), energy intake (kcal/day) 4) CT: computed tomography 5) ALT: alanine transferase 6) AST: aspartate transferase 7) GGT: glutamyl transferase 8) HOMA-IR: homeostasis model assessment of insulin resistance ab: Different alphabet letters within a row represent significant difference (
1) BMI: body mass index 2) Adjusted for age (years) and energy intake (kcal/day) 3) CT: computed tomography 4) HOMA-IR: homeostasis model assessment of insulin resistance **:
1) Adjusted for age(years), sex, smoking (no smoking, previous smoking. current smoking), drinking(no drinking, 1~4 times/month, >=5 times/month), physical activity(rarely, 1~2 times/week, >=3 times/week), energy intake (kcal/day) 2) MS : Metabolic syndrome *:

 KSCN
KSCN
 PubReader
PubReader Cite
Cite


