Search
- Page Path
- HOME > Search
Research Articles
- [English]
- Factors associated with malnutrition in demented and non-demented elderly residing in the community of Korea: a cross-sectional descriptive and analytical study
- Jinhee Kwon, Jung Hee Kim, Hyeonjin Jeong, Jung Suk Lee
- Korean J Community Nutr 2024;29(5):359-371. Published online October 31, 2024
- DOI: https://doi.org/10.5720/kjcn.2024.00013

-
 Abstract
Abstract
 PDF
PDF - Objectives
This study aimed to investigate and compare factors associated with malnutrition according to the presence or absence of dementia in community-dwelling elderly people.
Methods
Needs assessment data from 311 long-term care insurance (LTCI) recipients (dementia group 203; non-dementia group 108) that participated in the second pilot program of the integrated care model in community care settings under the Korean LTCI system were used. Descriptive statistical analysis, independent t-test, and analysis of variance were conducted on the sociodemographic characteristics, health and functional status, and nutritional status of the dementia and non-dementia groups. Logistic regression analysis was conducted to identify factors associated with malnutrition in the dementia and non-dementia groups.
Results
Malnutrition occurred in 33.5% and 26.9% of participants in the dementia and non-dementia groups, respectively. In the dementia group, living with family rather than living alone (odds ratio [OR]: 3.81; 95% confidence interval [CI]: 1.50–9.66; P = 0.031), increase in Korean Activities of Daily Living (K-ADL) score (OR: 1.35; 95% CI: 1.17–1.55; P < 0.001), and increase in the Neuropsychiatric Inventory-Questionnaire score (OR: 1.02; 95% CI: 1.01–1.03; P = 0.005) were associated with a higher risk of malnutrition. In the non-dementia group, the risk of malnutrition increased as the K-ADL score increased (OR: 1.20; 95% CI: 1.04–1.39; P = 0.011) and in the depressed group (OR: 2.84; 95% CI: 1.04–7.74; P = 0.042).
Conclusions
The study results confirmed the necessity of nutritional management for community-dwelling LTCI recipients. When developing a nutritional management program, considering the differences in factors related to malnutrition between the dementia and non-dementia groups is important. This study proposes policies for improving the LTCI system in terms of nutritional management and the utilization of community resources.
- 1,963 View
- 68 Download

- [Korean]
- Nutritional status of North Koreans and related perceptions among South Korean adults
- Youngmin Nam, Jihyun Yoon
- Korean J Community Nutr 2024;29(4):288-303. Published online August 31, 2024
- DOI: https://doi.org/10.5720/kjcn.2024.00006
-
 Abstract
Abstract
 PDF
PDF - Objectives
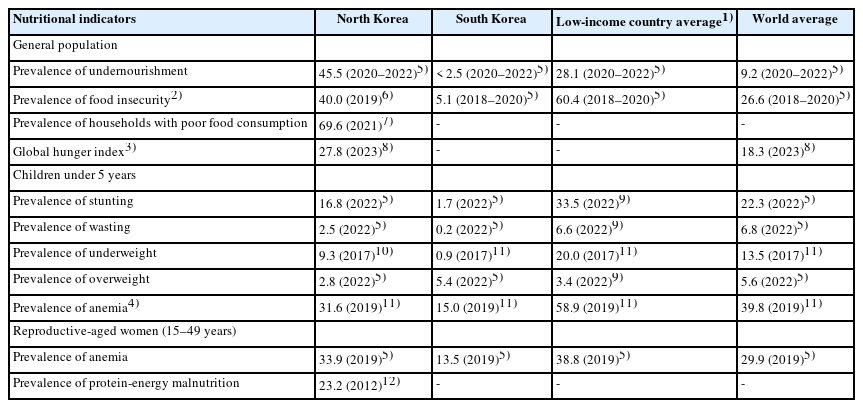
North Koreans have been facing chronic food shortages and malnutrition. This study examined the nutritional status of North Koreans and the perceptions of South Korean adults regarding their nutritional status.
Methods
The nutritional status was examined using nutritional indicators for the general population, children, and reproductive-aged women in North Korea. An online survey was conducted among 1,000 South Korean adults aged 19–69 years to investigate their perceptions regarding the nutritional status of North Koreans.
Results
Although the nutritional status of children in North Korea has consistently improved, significant progress in the general population and reproductive-aged women in the country remains elusive. The prevalence of malnutrition among North Korean children has decreased to a level that is not considered severe based on international standards, although it shows a substantial difference from that among South Korean children. The prevalence of undernourishment and food insecurity in North Korea remains over 40%. South Korean adults perceive the nutritional status of North Koreans as being more severe than it is in reality. Notably, a significant inconsistency exists between the perceived and actual nutritional status of North Korean children, with over 95% of South Korean adults perceiving North Korean children’s malnutrition as being more severe than it actually is. Moreover, South Korean adults in their 20s to 40s tended to perceive the nutritional status of North Koreans as being more severe than those in their 50s to 60s did.
Conclusions
The nutritional status of North Koreans is a matter of concern. The disparity between South Koreans’ perceptions of the nutritional status of North Koreans and the actual status highlights the need for accurate information dissemination to effectively address malnutrition in North Korea. These efforts could be instrumental in enhancing public awareness and fostering social consensus on food aid and nutritional support programs for North Korea.
- 3,727 View
- 68 Download

- [English]
- Nutritional status and dietary behavior of North Korean adolescent refugees based on Nutrition Quotient for Korean adolescents: a preliminary study
- Young Goh, Seong-Woo Choi, So-Yeong Kim, Jeong-Hwa Choi
- Korean J Community Nutr 2023;28(1):1-10. Published online February 28, 2023
- DOI: https://doi.org/10.5720/kjcn.2023.28.1.1
-
 Abstract
Abstract
 PDF
PDF - Objectives
This study aimed to investigate the nutritional status and dietary behavior of adolescents from North Korean refugee (NKR) families residing in South Korea (SK), who are known to be at a higher risk of malnutrition due to their lower socioeconomic status and facing other psychological challenges.
Methods
A total of 178 adolescents (91 males and 87 females) from NKR families were included in the analysis, and their demographic details such as age, birthplace, parental nationality, and duration of their settlement in SK were collected through questionnaires. Anthropometric measurements were also taken to determine their growth and nutritional status according to the 2017 Korean National Growth Charts for children and adolescents. The study used the Nutrition Quotient for Korean Adolescents (NQ-A) questionnaire to assess the dietary behavior of the participants.
Results
Approximately 11.8% and 10.1% of participants were identified with malnutrition and obesity, respectively. The total mean score for the NQ-A was 50.1. The mean scores for the individual factors of balance, diversity, moderation, environment, and practice were 49.2, 44.7, 43.8, 51.2, and 61.5, respectively. Approximately 47.2% of participants had a low NQ-A grade. However, there was no significant difference in the NQ-A scores according to their nutritional status or duration of time in SK.
Conclusions
Adolescents from NKR families exhibited both malnutrition and obesity. However, their dietary behavior, as assessed using the NQ-A, did not vary with their nutritional status. The unique challenges and related dietary behavior of North Korean adolescent refugees should be taken into consideration, when developing targeted strategies for nutritional education and health management programs.
- 1,813 View
- 24 Download

- [Korean]
- [Republished study] Assessing Nutritional Status in Outpatients after Gastric Cancer Surgery: A Comparative Study of Five Nutritional Screening Tools
- Jae Won Cho, Jiyoung Youn, Min-Gew Choi, Mi Young Rha, Jung Eun Lee
- Korean J Community Nutr 2022;27(3):205-222. Published online June 30, 2022
- DOI: https://doi.org/10.5720/kjcn.2022.27.3.205
-
 Abstract
Abstract
 PDF
PDF - Objectives
This study examined the characteristics of patients according to nutritional status assessed by five nutritional screening tools: Patient-Generated Subjective Global Assessment (PG-SGA), NUTRISCORE, Nutritional Risk Index (NRI), Prognostic Nutritional Index (PNI), and Controlling Nutritional Status (CONUT) and to compare the agreement, sensitivity, and specificity of these tools.
Methods
A total of 952 gastric cancer patients who underwent gastrectomy and chemotherapy from January 2009 to December 2012 were included. The patients were categorized into malnutrition and normal status according to five nutritional screening tools one month after surgery. The Spearman partial correlation, Cohen’s Kappa coefficient, the area under the curve (AUC), sensitivity, and specificity of each two screening tools were calculated.
Results
Malnutrition was observed in 86.24% of patients based on the PG-SGA and 85.82% based on the NUTRISCORE. When NRI or CONUT were applied, the proportions of malnutrition were < 30%. Patients with malnutrition had lower intakes of energy and protein than normal patients when assessed using the PG-SGA, NUTRISCORE, or NRI. Lower levels of albumin, hemoglobin, total lymphocyte count, and total cholesterol and longer postoperative hospital stays were observed among patients with malnutrition compared to normal patients when NRI, PNI, or CONUT were applied. Relatively high agreement for NUTRISCORE relative to PG-SGA was found; the sensitivity was 90.86%, and the AUC was 0.78. When NRI, PNI, and CONUT were compared, the sensitivities were 23.72% for PNI relative to NRI, 44.53% for CONUT relative to NRI, and 90.91% for CONUT relative to PNI. The AUCs were 0.95 for NRI relative to PNI and 0.91 for CONUT relative to PNI.
Conclusions
NUTRISCORE had a high sensitivity compared to PG-SGA, and CONUT had a high sensitivity compared to PNI. NRI had a high specificity compared to PNI. This relatively high sensitivity and specificity resulted in 77.00% agreement between PNI and CONUT and 77.94% agreement between NRI and PNI. Further cohort studies will be needed to determine if the nutritional status assessed by PG-SGA, NUTRISCORE, NRI, PNI, and CONUT predicts the gastric cancer prognosis. -
Citations
Citations to this article as recorded by- Report on the Current Trend of Commercial Enteral/Parenteral Nutrition in Outpatient
Hyun Ji Lee, Hyo Jung Park, Seon Young Chung, Myung Sook Min, Ok Soon Jeong, Ja Kyung Min
Journal of Korean Society of Health-System Pharmacists.2023; 40(2): 211. CrossRef
- Report on the Current Trend of Commercial Enteral/Parenteral Nutrition in Outpatient
- 1,359 View
- 27 Download
- 1 Crossref

- [Korean]
- Assessing Nutritional Status in Outpatients after Gastric Cancer Surgery : A Comparative Study of Five Nutritional Screening Tools
- Jae Won Cho, Jiyoung Youn, Min-Gew Choi, Mi Young Rha, Jung Eun Lee
- Korean J Community Nutr 2021;26(4):280-295. Published online August 31, 2021
- DOI: https://doi.org/10.5720/kjcn.2021.26.4.280
-
 Abstract
Abstract
 PDF
PDF - Objectives
This study aimed to examine the characteristics of patients according to their nutritional status as assessed by five nutritional screening tools: Patient-Generated Subjective Global Assessment (PG-SGA), NUTRISCORE, Nutritional Risk Index (NRI), Prognostic Nutritional Index (PNI), and Controlling Nutritional Status (CONUT) and to compare the agreement, sensitivity, and specificity of these tools. Methods: A total of 952 gastric cancer patients who underwent gastrectomy and chemotherapy from January 2009 to December 2012 at the Samsung Medical Center were included. We categorized patients into malnourished and normal according to the five nutritional screening tools 1 month after surgery and compared their characteristics. We also calculated the Spearman partial correlation, Cohen’s Kappa coefficient, the area under the curve (AUC), sensitivity, and specificity of each pair of screening tools. Results: We observed 86.24% malnutrition based on the PG-SGA and 85.82% based on the NUTRISCORE among gastric cancer patients in our study. When we applied NRI or CONUT, however, the malnutrition levels were less than 30%. Patients with malnutrition as assessed by the PG-SGA, NUTRISCORE, or NRI had lower intakes of energy and protein compared to normal patients. When NRI, PNI, or CONUT were used to identify malnutrition, lower levels of albumin, hemoglobin, total lymphocyte count, total cholesterol, and longer postoperative hospital stays were observed among patients with malnutrition compared to those without malnutrition. We found relatively high agreement between PG-SGA and NUTRISCORE; sensitivity was 90.86% and AUC was 0.78. When we compared NRI and PNI, sensitivity was 99.64% and AUC was 0.97. AUC ranged from 0.50 to 0.67 for comparisons between CONUT and each of the other nutritional screening tools. Conclusions: Our study suggests that PG-SGA and NRI have a relatively high agreement with the NUTRISCORE and PNI, respectively. Further cohort studies are needed to examine whether the nutritional status assessed by PG-SGA, NUTRISCORE, NRI, PNI, and CONUT predicts the gastric cancer prognosis. -
Citations
Citations to this article as recorded by- Effects of Continuous Nutrition Care on Nutritional Status and Dietary Habits of Patients With Colorectal Cancer Receiving Adjuvant Chemotherapy After Surgery
Jina Son, Ha I Kang, Eun young Jung, Hae won Ryu, Kyung-Ha Lee
Clinical Nutrition Research.2023; 12(2): 99. CrossRef
- Effects of Continuous Nutrition Care on Nutritional Status and Dietary Habits of Patients With Colorectal Cancer Receiving Adjuvant Chemotherapy After Surgery
- 1,345 View
- 17 Download
- 1 Crossref

Original Articles
- [English]
- Effect of Active Nutrition Care on Underweight Elderly Patients Receiving Long-term Enteral Tube Feeding
- Hwa Young Yoon, Hye Kyeong Kim
- Korean J Community Nutr 2018;23(1):48-59. Published online February 28, 2018
- DOI: https://doi.org/10.5720/kjcn.2018.23.1.48
-
 Abstract
Abstract
 PDF
PDF - OBJECTIVES
This study was performed to investigate the effect of active nutrition care on feeding and nutritional status of elderly patients receiving long-term enteral tube feeding.
METHODS
Subjects included 77 elderly patients who had received enteral nutrition more than one week before admission. Nutrition care was provided to patients supplied less calories than required. Feeding intolerance was examined and managed every day and formula was adjusted to meet nutritional requirement during the first 3 months after admission. Patients were classified into under or over 80% of percent ideal body weight (PIBW) and medical records were used to compare changes in weight,, biochemical indices, and nutritional status during the study.
RESULTS
Weight, BMI, triglyceride and total cholesterol in blood, hemoglobin, and hematocrit levels were significantly lower in patients under 80% of the PIBW than in those over 80% of the PIBW at admission. The percentage of supply to required calories was also lower in patients under 80% of the PIBW. After 1 month of nutritional care, supplied volume of formula was significantly increased in patients under 80% of the PIBW. Weight, BMI, and PIBW were increased and there were no differences between groups after 6 months. In addition, the concentrations of triglyceride and total cholesterol in blood, hemoglobin, and hematocrit tended to increase in patients under 80% of the PIBW, leading to no difference between groups after 3 months.
CONCLUSIONS
Personalized active nutrition care is effective to increase weight and improve feeding and nutritional status in underweight elderly patients receiving longterm enteral nutrition. -
Citations
Citations to this article as recorded by- The Status of Enteral Nutrition Formula Use by Dietitians in Hospitals Within Busan and Gyeongnam Area
Haejin Kang, Minji Woo, Eunju Park, Yoo Kyoung Park
Clinical Nutrition Research.2022; 11(1): 9. CrossRef
- The Status of Enteral Nutrition Formula Use by Dietitians in Hospitals Within Busan and Gyeongnam Area
- 1,056 View
- 5 Download
- 1 Crossref

- [English]
- Nutritional Risk in Oncology Outpatients Receiving Chemotherapy
- Won Gyoung Kim, Mi Sun Park, Young Hee Lee, Dae Seog Heo
- Korean J Community Nutr 2008;13(4):573-581. Published online August 31, 2008
-
 Abstract
Abstract
 PDF
PDF - Although it is well known that cancer patients suffer from malnutrition, there are few published studies on malnutrition in outpatients receiving chemotherapy in Korea. This study aimed to evaluate nutritional risk in oncology outpatients receiving chemotherapy and to show the baseline data to set up nutritional management programs for cancer patients. This is a retrospective observational analysis on 1,962 patients referred for nutritional education before or during chemotherapy at Seoul National University Hospital Cancer Center from January 2006 to May 2007. According to a malnutrition screening tool, the proportion of patients having malnutrition risk was 23.0%. In the case of upper gastrointestinal cancer, more than 50% of patients were assessed as being at the risk of malnutrition. They showed more than 7% weight loss compared to their usual body weight and poor oral intake; energy intake was less than 100% of Basal Energy Expenditure (BEE) and protein intake was less than or equal to 0.77 g/kg/d. However, only 6.3% of breast cancer patients had risk of malnutrition and their oral intake was better; energy intake was 121% of BEE, and protein intake was 0.90 g/kg/d. Outpatients receiving chemotherapy had different nutritional risk depending on their cancer site. Nutritional management program should be conducted differently, depending on the cancer site and upper gastrointestinal cancer patients at high risk of malnutrition should basically have nutritional assessment and intervention.
- 268 View
- 5 Download

- [English]
- Development of Nutrition Screening Index for Hospitalized Patients
- Suan Kim, Soyeon Kim, Cheongmin Sohn
- Korean J Community Nutr 2006;11(6):779-784. Published online December 31, 2006
-
 Abstract
Abstract
 PDF
PDF - Several studies about hospital malnutrition have been reported that about more than 40% of hospitalized patients are having nutritional risk factors and hospital malnutrition presents a high prevalence. People in a more severe nutritional status ended up with a longer length of hospital stay and higher hospital cost. Nutrition screening tools identify individuals who are malnourished or at risk of becoming malnourished and who may benefit from nutritional support. For the early detection and treatment of malnourished hospital patients, few valid screening instruments for Koreans exist. Therefore, the aim of this study was to develop a simple, reliable and valid malnutrition screening tool that could be used at hospital admission to identify adult patients at risk of malnutrition using medical electrical record data. Two hundred and one patients of the university affiliated medical center were assessed on nutritional status and classified as well nourished, moderately or severely malnourished by a Patient-Generated subjective global assessment (PG-SGA) being chosen as the 'gold standard' for defining malnutrition. The combination of nutrition screening questions with the highest sensitivity and specificity at prediction PG-SGA was termed the nutrition screening index (NSI). Odd ratio, and binary logistic regression were used to predict the best nutritional status predictors. Based on regression coefficient score, albumin less than 3.5 g/dl, body mass index (BMI) less than 18.5 kg/m2, total lymphocyte count less than 900 and age over 65 were determined as the best set of NSI. By using best nutritional predictors receiver operating characteristic curve with the area under the curve, sensitivity and 1-specificity were analyzed to determine the best optimal cut-off point to decide normal or abnormal in nutritional status. Therefore simple and beneficial NSI was developed for identifying patients with severe malnutrition. Using NSI, nutritional information of the severe malnutrition patient should be shared with physicians and they should be cared for by clinical dietitians to improve their nutritional status.
- 335 View
- 8 Download

- [English]
- The Outcome of Nutrition Support of Surgery Patients with Hypermetabolic Severity by Total Parenteral Nutrition and Enteral Nutrition and Biochemical Data
- Miyong Rha, Eunmi Kim, Young Y Cho, Jeong Meen Seo, Haymie Choi
- Korean J Community Nutr 2006;11(2):289-297. Published online April 30, 2006
-
 Abstract
Abstract
 PDF
PDF - This study evaluated the nutrition intake and changes in laboratory data of surgery patients with hypermetabolic severity on nutrition support. From January 2002 to September 2002, 66 hospitalized surgery patients who had received enteral nutrition (EN, n=19) and total parenteral nutrition (TPN, n=47) for more than 7 days were prospectively and retrospectively recruited. The laboratory data was examined pre-operatively, and on the post-operative 1, 3, 7 day and at the time of discharge. The characteristics of the patients were examined for the hypermetabolic severity, The hypermetabolic scores were determined by high fever (> 38 degrees C), rapid breathing (> 30 breaths/min), rapid pulse rate (> 100 beats/min), leukocytosis (WBC>12,000/microliter), leukocytopenia (WBC<3,000/microliter), status of infection, inflammatory bowel disease, surgery and trauma. The scores for the hypermetabolic status were divided into three groups (mild 0-10, moderate 11-40, severe>41). According to the results of the study, 38.3% (n=23), 45.4% (n=30) and 19.6% (n=13) were in the mild, moderate, and severe groups, respectively. There was a decrease in the serum albumin level and weight loss according to the hypermetabolic severity. However, the white blood cells (WBC), fasting blood sugar (FBS), c-reactive protein (CRP), total bilirubin, GOT, and GPT increased. The nutritional intake was TPN (32.5 kcal/kg, protein 1.2 g/kg, fat 0.25 g/kg), EN (28.1 kcal/kg, protein 1.0 g/kg, fat 1.01 g/kg). The serum albumin, hemoglobin and cholesterol were higher in the EN group than in the TPN group. But the FBS, total bilirubin, GOT and GPT were higher in the TPN group than the EN group. In conclusion, there was a negative correlation between the changes in the laboratory data and the hypermetabolic severity. There was an increase in the number of metabolic complications in the TPN group.
- 262 View
- 2 Download

- [English]
- Effects of the APACHE III Score, Hypermetabolic Score on the Nutrition Status and Clinical Outcome of the Patients Administered with Total Parenteral Nutrition and Enteral Nutrition
- Miyong Rha, Eunmi Kim, Young Y Cho, Jeong Meen Seo, Haymie Choi
- Korean J Community Nutr 2006;11(1):124-132. Published online February 28, 2006
-
 Abstract
Abstract
 PDF
PDF - The aim of this study is to evaluate the clinical outcome. Between January 1, 2002 to September 30, 2002, we prospectively and retrospectively recruited 111 hospitalized patients who received Enteral Nutrition (ENgroup n = 52) and Total Parenteral Nutrition (TPNgroup n = 59) for more than seven days. The factors of clinical outcomes are costs, incidences of in-fection, lengths of hospital stay, and changes in weight. The characteristics of patients were investigated, which included nutritional status, disease severity (APACHE III score) and hypermetabolic severity (hypermetabolic score). Hypermeta-bolic scores were determined by high fever (>38 degrees C), rapid breathing (>30 breaths/min), rapid pulse rate (>100 beats/min), leukocytosis (WBC > 12000 mm3), leukocytopenia (WBC < 3000 mm3), status of infection, inflammatory bowel disease, surgery and trauma. There was a positive correlation between hypermetabolic score and length of hospital stay (ICU), medical cost, weight loss, antibiotics adjusted by age while APACHE III score did not show correlation to clinical outcome. Medical cost was higher by 18.2% in the TPN group than the EN group. In conclusion, there was a strong negative correlation between the clinical outcome (cost, incidence of infection, hospital stay) and hypermetabolic score. Higher metabolic stress caused more malnutrition and complications. For nutritional management of patients with malnutrition, multiple factors, including nutritional assessment, and evaluation of hypermetabolic severity are needed to provide nutritional support for critically ill patients.
- 286 View
- 0 Download

- [English]
- Nutritional Status of Hospitalized Geriatric Patients Using by the Mini Nutritional Assessment
- Su Hyun Chung, Cheong Min Sohn
- Korean J Community Nutr 2005;10(5):645-653. Published online October 31, 2005
-
 Abstract
Abstract
 PDF
PDF - The prevalence of undernutrition in hospital populations is known to be high. The presence of malnutrition is associated with depression, infections, sarcopaenia, falls, fractures, reduced autonomy and increased mortality. This study specifically examined the prevalence of malnutrition in patients aged 65 or older at the time of admission as determined by the Mini Nutritional Assessment (MNA) which has been a frequently used nutritional risk screening tools in detecting undernutrition in old people. This study was done for one hundred eight hospitalized geriatric patients in Seoul National University Bundang Hospital, Seoul, Korea. On admission baseline history, anthropometrics measurements, laboratory data and nutritional status by MNA were assessed. Length of hospital stay was obtained by reviewing medical charts. We used one-way analysis of variance to compare the differences in variables. Spearman's rank correlation coefficients were calculated for associations between MNA and variables. On admission, 22.3% of patients were malnourished and 40.7% were at risk of malnutrition according to the MNA. Percent of ideal body weight, anthropometrics data, albumin, and hemoglobin were lower in the malnourished patients (p < 0.05). The malnourished patients stayed in the hospital 7.3 days longer, as compared with well nourished patients (p < 0.05). Percent of ideal body weight, albumin, hemoglobin and total cholesterol were correlated inversely with nutritional status according to MNA (p < 0.05). MNA can be used for nutritional assessment in Korean old people, because MNA significantly correlated with other nutritional assessment parameters, such as, anthropometric and laboratory data in hospitalized geriatric patients. The high prevalence of malnutrition in the elderly was observed and the presence of malnutrition on admission predicted a significant increase in the length of hospital stay in this study. Therefore further studies are needed to determine whether nutritional interventions in old people with low MNA scores can improve clinical outcomes during the hospital course.
- 266 View
- 2 Download


 KSCN
KSCN

 First
First Prev
Prev



