Search
- Page Path
- HOME > Search
Research Article
- [English]
- Self-reported weight change and diet quality in relation to metabolic syndrome among Korean cancer survivors: a cross-sectional study using the Korea National Health and Nutrition Examination Survey 2019–2021
- Hye Won Kim, Ji-Myung Kim
- Korean J Community Nutr 2025;30(5):341-351. Published online October 31, 2025
- DOI: https://doi.org/10.5720/kjcn.2025.00241
-
 Abstract
Abstract
 PDF
PDF - Objectives
Using data from the 2019‒2021 Korea National Health and Nutrition Examination Survey, we examined the association between dietary quality and metabolic syndrome by self-reported weight change among adult Korean cancer survivors.
Methods
We analyzed 340 cancer survivors (≥ 5 years post-diagnosis) by one-year weight change (stable, loss, and gain). Dietary quality was assessed using the Korean Healthy Eating Index (KHEI), and metabolic syndrome was defined according to standard criteria. Relative risks (RR) were estimated using a modified Poisson regression.
Results
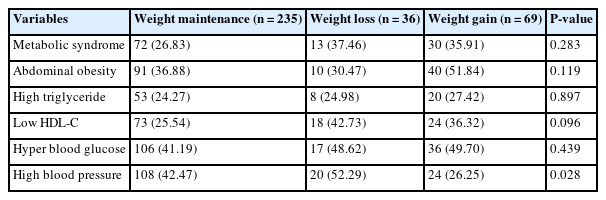
The weight loss group was older than the weight gain group (P < 0.001). Females were more prevalent in the loss and gain than in the maintenance group (P = 0.008). Hypertension prevalence was highest in the loss and lowest in the gain group (P = 0.028); other risk factors were similar. The gain group had the highest body mass index (P = 0.011). KHEI scores were highest in the maintenance (66.59 ± 0.76) and lowest in the gain group (60.42 ± 1.77; P = 0.006), with significantly lower whole grain (P = 0.036) and fruit intake (P = 0.014). Compared with the maintenance group, the gain group demonstrated higher risks of metabolic syndrome (RR: 2.07, 95% confidence interval [CI]: 1.40–3.06; P < 0.001), abdominal obesity (RR: 1.93, 95% CI: 1.36–2.74; P < 0.001), and impaired fasting glucose (RR: 1.70, 95% CI: 1.23–2.34; P < 0.01). Within the gain group, participants in the lowest KHEI quartile had increased risks of metabolic syndrome (RR: 2.81, 95% CI: 1.06–7.43; P < 0.05) and hypertriglyceridemia (RR: 7.29, 95% CI: 1.54–34.61; P < 0.05).
Conclusion
Accordingly, weight change and dietary quality may critically affect the metabolic health of cancer survivors. Lifestyle management, including weight control and tailored diets, may help prevent metabolic disorders and support long-term health.
- 659 View
- 15 Download

Original Article
- [English]
- Eating and Exercise Behaviors of University Students by Weight Change Status
- Seolhyang Baek, Eunjeong Kim
- Korean J Community Nutr 2009;14(4):374-382. Published online August 31, 2009
-
 Abstract
Abstract
 PDF
PDF - Young adults are likely to start a new life style which may cause weight gain or obesity since leaving their parents for higher education or university. Whilst young people are slim in general, it is common to see them trying to manage their weight. Few studies have been carried out in Korea to support those changes in lifestyle that can result in weight gain in early adulthood. This study aims to identify prevalence of dieting as well as factors inducing weight gain among university students under unrestricted living conditions. A total of 99 university students were enrolled and asked to complete a questionnaire over a 3-day study period from June to September, 2008. T-test and chi-square-test were applied to compare each behavior between weight gainers and maintainers. Logistic regression was also used for further analysis. Half of the participants used 'eat less' and 'exercise' as a way of dieting, and weight gainers tried to control their weight significantly more than weight maintainers. Most participants were engaged in very little exercise and were more likely to watch TV and use a computer. The time of lunch was proven as the only factor to predict weight change in the participants. As a result of this study, an intervention to promote exercise with friends or as a group is required to makeup for the lack of exercise among young adults. Further studies are also necessary to investigate how each meal time a day relates to the amount of food eaten.
- 300 View
- 2 Download


 KSCN
KSCN
 First
First Prev
Prev



