Articles
- Page Path
- HOME > Korean J Community Nutr > Volume 25(4); 2020 > Article
- Research Article
- Qualitative Study of Compliance with Nutritional Management in Colorectal Cancer Patient Undergoing Chemotherapy
- Heejung Park, Hyonson Kil, Wookyoun Cho
-
Korean Journal of Community Nutrition 2020;25(4):303-316.
DOI: https://doi.org/10.5720/kjcn.2020.25.4.303
Published online: August 31, 2020
2Graduate student, Department of Clinical Nutrition, Gachon University Graduate School of Professional Therapy, Seongnam, Korea
3Professor, Department of Food & Nutrition, Gachon University, Seongnam, Korea
-
Corresponding author:
Wookyoun Cho,
Email: wkcho@gachon.ac.kr
- 1,274 Views
- 22 Download
- 1 Crossref
- 0 Scopus
Abstract
Objective
The nutritional status of cancer patients undergoing chemotherapy is closely related to the compliance of nutrition education. However, as chemotherapy is conducted repeatedly, compliance with nutrition management is lowered, leading to malnutrition. Malnutrition is related directly to the quality of life after surgery in cancer patients. Therefore, this study examined the factors related to compliance with nutrition management during chemotherapy.
Methods
In this study, five subjects with colorectal cancer undergoing adjuvant chemotherapy were interviewed in-depth using the Giorgi study method. The contents of the nutrition education visits and in-depth interviews were transcribed in the language of the subject after recording, and the appropriateness of the data was improved by reflecting the subject’s actions and facial expressions.
Results
After conducting the in-depth interviews for each subject, the experience of the subject’s diet and adjuvant chemotherapy was drawn into two domains, six elements, and 26 sub-elements. In the cognitive domain, the patients experienced physical and psychological changes, and the need for nutrition management was recognized by analyzing the dietary causes of the diseases. In the domain of practice, a knowing-doing gap was formed, unlike the patient’s will. Factors that inhibited compliance with nutritional management included digestive problems, sensory changes, loss of appetite, and social interaction stress.
Conclusions
Dietary management is very important for patients receiving periodic anticancer therapy, and step-by-step training and personal monitoring based on the chemotherapy order is necessary to maintain the patient’s will and social and environmental support.
Published online Aug 31, 2020.
https://doi.org/10.5720/kjcn.2020.25.4.303
Qualitative Study of Compliance with Nutritional Management in Colorectal Cancer Patient Undergoing Chemotherapy
Abstract
Objectives
The nutritional status of cancer patients undergoing chemotherapy is closely related to the compliance of nutrition education. However, as chemotherapy is conducted repeatedly, compliance with nutrition management is lowered, leading to malnutrition. Malnutrition is related directly to the quality of life after surgery in cancer patients. Therefore, this study examined the factors related to compliance with nutrition management during chemotherapy.
Methods
In this study, five subjects with colorectal cancer undergoing adjuvant chemotherapy were interviewed in-depth using the Giorgi study method. The contents of the nutrition education visits and in-depth interviews were transcribed in the language of the subject after recording, and the appropriateness of the data was improved by reflecting the subject's actions and facial expressions.
Results
After conducting the in-depth interviews for each subject, the experience of the subject's diet and adjuvant chemotherapy was drawn into two domains, six elements, and 26 sub-elements. In the cognitive domain, the patients experienced physical and psychological changes, and the need for nutrition management was recognized by analyzing the dietary causes of the diseases. In the domain of practice, a knowing-doing gap was formed, unlike the patient's will. Factors that inhibited compliance with nutritional management included digestive problems, sensory changes, loss of appetite, and social interaction stress.
Conclusions
Dietary management is very important for patients receiving periodic anticancer therapy, and step-by-step training and personal monitoring based on the chemotherapy order is necessary to maintain the patient's will and social and environmental support.
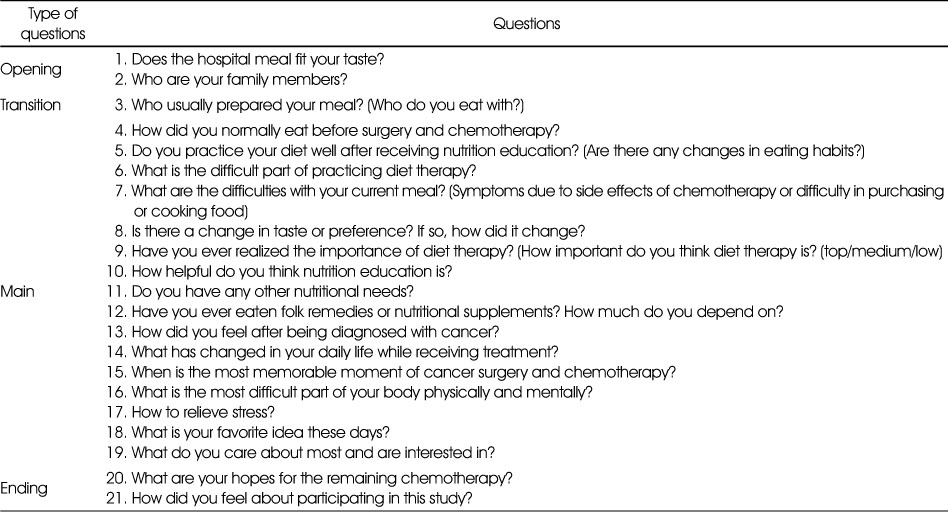
Table 1
List of questions
Table 2
Participants' characteristics
Table 3
Experience of colorectal patients with chemotherapy related to dietary management
References
-
Statistics Korea. Cancer registration statistics [internet]. Statistics Korea. 2017 [cited 2020 Mar 19].Available from: http://kosis.kr/eng/statisticsList/statisticsListIndex.do?menuId=M_
01_ 01&vwcd=MT_ ETITLE&parmTabId=M_ 01_ 01&statId=1997018&themaId=#SelectStatsBoxDiv.
-
-
Mizota Y, Kanemitsu Y, Tsukamoto S, Shida D, Ochiai H, Yamamoto S. ROK study-C (Rainbow of KIBOU studycolorectum): a colorectal cancer survivor cohort study on food, nutrition, physical activity, psychosocial factors and its influences on colorectal cancer recurrence, survival and quality of life in Japan. BMC Cancer 2018;18(1):953–961.
-
-
Hong KY, Choi YJ, Yan WQ, Lim HS, Chyun JH. Study on the improvement of dietary life of cancer patients during treatment by nutrition counseling. Korean J Community Nutr 2016;21(1):93–101.
-
-
Matsumoto K, Takahashi M, Sato K, Osaki A, Takano T, Naito Y. A double-blind, randomized, multicenter phase 3 study of palonosetron vs granisetron combined with dexamethasone and fosaprepitant to prevent chemotherapy-induced nausea and vomiting in patients with breast cancer receiving anthracycline and cyclophosphamide. Cancer Med 2020;9(10):3319–3327.
-
-
Mardas M, Madry R, Stelmach-Mardas M. Link between diet and chemotherapy related gastrointestinal side effects. Contemp Oncol (Pozn) 2017;21(2):162–167.
-
-
Ravasco P. Nutrition in cancer patients. J Clin Med 2019;8(8):1211–1223.
-
-
Hébuterne X, Lemarié E, Michallet M, de Montreuil CB, Schneider SM, Goldwasser F. Prevalence of malnutrition and current use of nutrition support in patients with cancer. J Parenter Enteral Nutr 2014;38(2):196–204.
-
-
Demark-Wahnefried W, Morey MC, Sloane R, Snyder DC, Miller PE, Hartman TJ. Reach out to enhance wellness home-based diet-exercise intervention promotes reproducible and sustainable long-term improvements in health behaviors, body weight, and physical functioning in older, overweight/obese cancer survivors. J Clin Oncol 2012;30(19):2354–2361.
-
-
Rock CL, Flatt SW, Byers TE, Colditz GA, Demark-Wahnefried W, Ganz PA. Results of the exercise and nutrition to enhance recovery and good health for You (ENERGY) trial: a behavioral weight loss intervention in overweight or obese breast cancer survivors. J Clin Oncol 2015;33(28):3169–3176.
-
-
Langius JA, Zandbergen MC, Eerenstein SE, van Tulder MW, Leemans CR, Kramer MH. Effect of nutritional interventions on nutritional status, quality of life and mortality in patients with head and neck cancer receiving (chemo) radiotherapy: a systematic review. Clin Nutr 2013;32(5):671–678.
-
-
Van Blarigan EL, Fuchs CS, Niedzwiecki D, Zhang S, Saltz LB, Mayer RJ. Association of survival with adherence to the American cancer society nutrition and physical activity guidelines for cancer survivors after colon cancer diagnosis: The CALGB 89803/Alliance trial. JAMA Oncol 2018;4(6):783–790.
-
-
Min HS, Hwang WH. The effects of nutritional education program on nausea and vomiting, anorexia, food intake, and nutritional status of GI cancer patients undergoing chemotherapy. Asian Oncol Nurs 2010;10(1):38–47.
-
-
Custódio ID, Marinho Eda C, Gontijo CA, Pereira TS, Paiva CE, Maia YC. Impact of chemotherapy on diet and nutritional status of women with breast cancer: a prospective study. PLoS One 2016;11(6):e0157113
-
-
Yang YH. Anorexia, nausea and vomiting, and food intake patterns in patients on chemotherapy. J Korean Acad Fundam Nurs 2004;11(2):177–185.
-
-
Park JS. A qualitative case study on the coping experiences of cancer survivors in their middle years. Health Soc Welfare Rev 2017;37(2):525–561.
-
-
Shin KR. Criteria for critique of qualitative nursing research. J Korean Acad Nurs 1996;26(2):497–506.
-
-
Kim BH, Kim KJ, Park IS, Lee KJ, Kim JK, Hong JJ. A comparison of phenomenological research methodology. J Korean Acad Nurs Adm 1999;29(6):1208–1220.
-
-
Giorgi A. In: Phenomenology and psychological research. Pittsburgh: Duquesne University Press; 1985.
-
-
Oh PJ, Lim SY. Change of cancer symptom, depression and quality of life based on phases of chemotherapy in patients with colorectal or stomach cancer: a prospective study. Korean J Adult Nurs 2017;29(3):313–322.
-
-
Kim JH, Choi KS, Kim TW, Hong YS. Quality of life in colorectal cancer patients with chemotherapy-induced peripheral neuropathy. J Korean Oncol Nurs 2011;11(3):254–262.
-
-
Alkhaldy AA, Aljahdli ES, Mosli MH, Jawa HA, Alsahafi MA, Qari YA. Adherence to the Saudi dietary guidelines and its relation to colorectal polyps: A university hospital-based study. J Taibah Univ Med Sci 2019;15(1):25–31.
-
-
Jeong GH, Kim KH, Kwak YH. Quality of life in colorectal cancer patients according to the severity of symptom clusters classification. Asian Oncol Nurs 2014;14(2):74–83.
-

 KSCN
KSCN



 Cite
Cite


