- [Korean]
-
Impact of a public health center nutrition education program on patients with type 2 diabetes in a primary care-based chronic disease management project: a pilot intervention study
-
Haerim Yang, Yoo Kyoung Park, Ji-hyun Lee, Hee-Sook Lim, Heejoon Baek, Hyejin Lee, Haeran Park, Pyunghwa Lee, Jooyoun Chung, Won Gyoung Kim
-
Korean J Community Nutr 2024;29(6):492-503. Published online December 31, 2024
-
DOI: https://doi.org/10.5720/kjcn.2024.00018
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Objectives
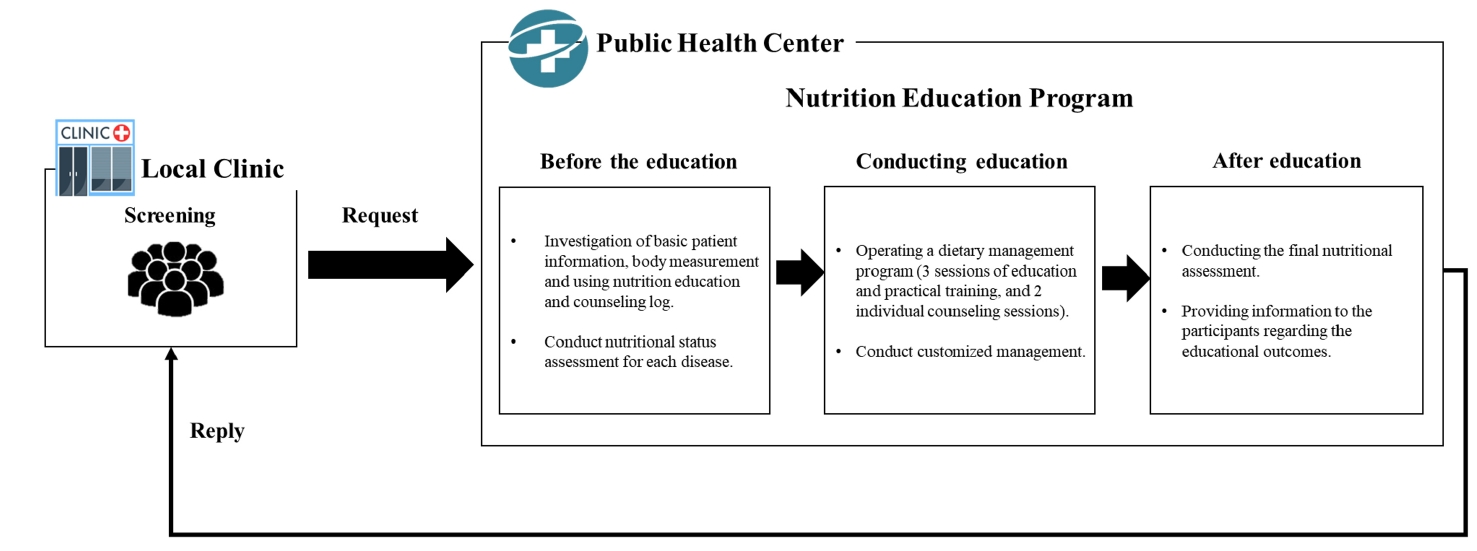
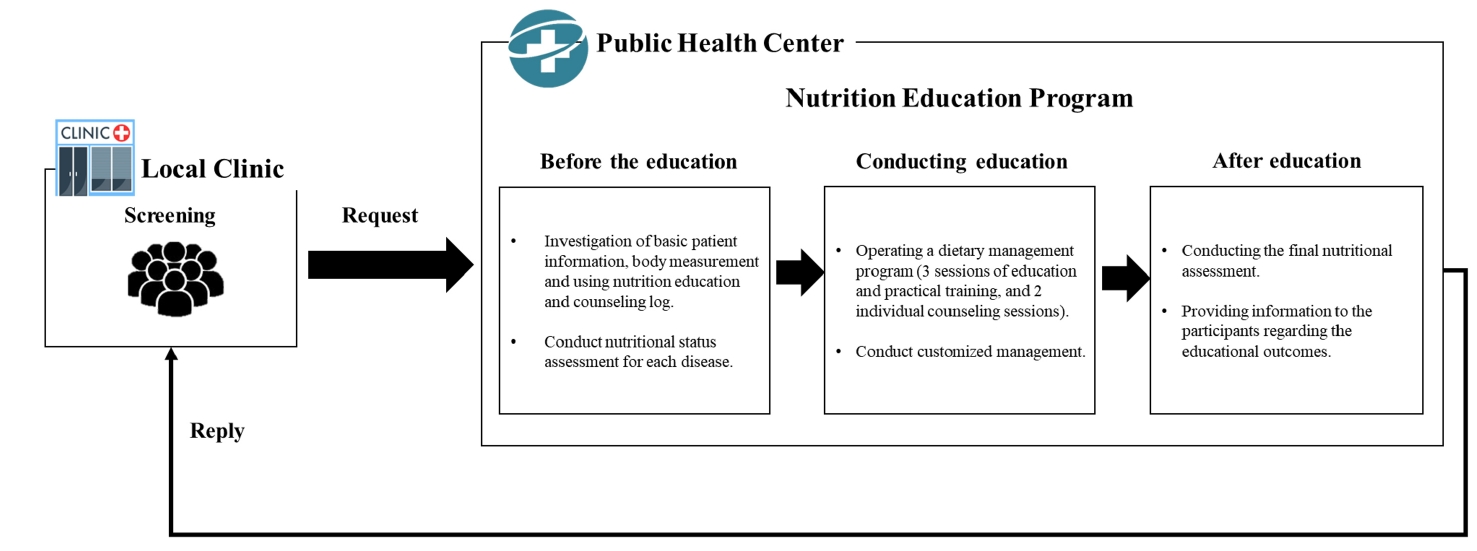
We investigated the impact of an advanced “Nutrition Education Program” on patients with Diabetes mellitus, type 2 from public health centers enrolled in a primary health care-based chronic disease management project. This 12-week dietary management program was developed by the Korea Health Promotion and Development Institute. We assessed if this program improved glycemic control and other health indicators through dietary and nutritional improvements.
Methods
Seventeen patients with Diabetes mellitus type 2 were enrolled in the “Nutrition Education Program.” These patients were referred to public health centers for lifestyle management based on physician assessments at local clinics that were participating in a pilot project on primary health care-based chronic disease management. The participants attended the program comprising face-to-face basic, in-depth, and practical training sessions at the health center during the third, fifth, and seventh weeks, respectively. Anthropometric measurements, body composition analysis, blood biochemical characteristics, nutritional knowledge, and self-efficacy evaluation were performed before and after the program. Data were analyzed using SPSS ver. 28.0.
Results
The mean age of the participants was 62 years, and most participants were female (14, 82.4%). No significant changes in patients’ anthropometric measurements or body composition were observed after the training. However, significant reductions were observed in the blood biochemical characteristics, including glycated hemoglobin, total cholesterol, and low-density lipoprotein levels. Additionally, patients’ nutritional knowledge and self-efficacy scores increased significantly.
Conclusions
The “Nutrition Education Program” helped in improving glycemic control and other health indicators in patients with Diabetes mellitus type 2. Further research is required to objectively confirm the long-term and sustained effects of the program in a controlled study.
Trial Registration
Clinical Research Information Service Identifier: KCT0010010
- [English]
-
Effect of a Worksite-based Dietary Intervention Program for the Management of Metabolic Syndrome
-
Hye Jin Kim, Injoo Choi, Won Gyoung Kim, Kana Asano, Jeongmin Hong, Young Min Cho, Jihyun Yoon
-
Korean J Community Nutr 2016;21(3):237-246. Published online June 30, 2016
-
DOI: https://doi.org/10.5720/kjcn.2016.21.3.237
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader
- OBJECTIVES
To investigate the effect of a worksite-based dietary intervention program for the management of metabolic syndrome (MS) among male employees.
METHODS
A dietary intervention program combining individual and environmental approach was implemented targeting white-collar employees at a worksite located in Seoul for 10 weeks. Out of 104 employees having agreed to participate in the program, those having three or more out of five components of MS and having two components, including a waist circumference component were classified into "the high risk group" (n=41) and received group nutrition education and individual nutrition counseling three times each. The rest of the study subjects were considered as "the low risk group" (n=63). The food environment at the worksite, where both the high and low risk groups were exposed, was changed to promote healthy eating. Physical data including MS components were collected and a questionnaire on dietary behaviors was administered before and after the intervention. The data from the high risk group (n=17) and the low risk group (n=20), excluding the subjects ineligible for or failed to complete the study (n=67), were analyzed. The difference before and after intervention was tested for significance by Wilcoxon signed-rank tests.
RESULTS
Weight, body mass index (BMI), waist circumference, blood pressure, HDL-cholesterol, and HbA1c and the healthy dietary practice score improved significantly after intervention in the high risk group. The median number of MS components decreased significantly from 3.0 to 1.0 in the high risk group. In the low risk group, only HbA1c significantly decreased. Conclusions: The 10-week worksite-based dietary intervention program combining individual and environmental approach was found to be effective for managing MS of male employees.
CONCLUSIONS
The 10-week worksite-based dietary intervention program combining individual and environmental approach was found to be effective for managing MS of male employees.
-
Citations
Citations to this article as recorded by  - A cohort study of the effects of social support on cerebral cardiovascular disease in subjects with metabolic syndrome
Sung-Kyung Kim, Yong Whi Jeong, Dae Ryong Kang, Jang Young Kim, Hunju Lee, Sang-baek Koh, Yoshihiro Fukumoto
PLOS ONE.2024; 19(7): e0305637. CrossRef - Salutogenesis intervention improves cardio‐cerebrovascular health in at‐risk office workers: A quasi‐experimental study
Ji Hyun Moon, Hosihn Ryu
Public Health Nursing.2024; 41(4): 690. CrossRef - Process evaluation of a mobile healthcare program among employees with overweight and obesity: a 12-week intervention study investigating the role of engagement
Imhuei Son, Jiyoun Hong, Young Hee Han, Bo Jeong Gong, Meng Yuan Zhang, Woori Na, Cheongmin Sohn, Taisun Hyun
Korean Journal of Community Nutrition.2023; 28(6): 466. CrossRef - Facilitators and barriers to achieving dietary and physical activity goals: focus group interviews with city bus drivers and counseling dietitians
Yongmin Jo, Suhyeun Cho, Young-Hee Han, Taisun Hyun
Korean Journal of Community Nutrition.2023; 28(5): 376. CrossRef - Effectiveness of a mobile health intervention on weight loss and dietary behavior changes among employees with overweight and obesity: a 12-week intervention study investigating the role of engagement
Imhuei Son, Jiyoun Hong, Young-Hee Han, Bo Jeong Gong, Meng Yuan Zhang, Woori Na, Cheongmin Sohn, Taisun Hyun
Korean Journal of Community Nutrition.2023; 28(2): 141. CrossRef - Predictors of Health Promotion Behaviors Among Working Adults at Risk for Metabolic Syndrome
Sungwon Park, Min Kyeong Jang, Chang Gi Park, Oi Saeng Hong
Nursing Research.2022; 71(4): 275. CrossRef - Inverse association of improved adherence to dietary guidelines with metabolic syndrome: the Seoul Metabolic Syndrome Management program
Dongwoo Ham, YoungYun Cho, Mi-Suk Park, Yun-Sug Park, Sun-Young Kim, Hye-Min Seol, Yoo Mi Park, Sunok Woo, Hyojee Joung, Do-Sun Lim
Nutrition Research and Practice.2020; 14(6): 621. CrossRef - The Effect of Community-based Health Intervention Program to Improve Metabolic Disease in Jeju Island
Woo Jin Kim, Sang Hoon Kim, Shin Young Park
The Korean Journal of Clinical Laboratory Science.2018; 50(3): 297. CrossRef
-
667
View
-
1
Download
-
8
Crossref
- [English]
-
Nutritional Risk in Oncology Outpatients Receiving Chemotherapy
-
Won Gyoung Kim, Mi Sun Park, Young Hee Lee, Dae Seog Heo
-
Korean J Community Nutr 2008;13(4):573-581. Published online August 31, 2008
-
-
-
 Abstract Abstract
 PDF PDF
- Although it is well known that cancer patients suffer from malnutrition, there are few published studies on malnutrition in outpatients receiving chemotherapy in Korea. This study aimed to evaluate nutritional risk in oncology outpatients receiving chemotherapy and to show the baseline data to set up nutritional management programs for cancer patients. This is a retrospective observational analysis on 1,962 patients referred for nutritional education before or during chemotherapy at Seoul National University Hospital Cancer Center from January 2006 to May 2007. According to a malnutrition screening tool, the proportion of patients having malnutrition risk was 23.0%. In the case of upper gastrointestinal cancer, more than 50% of patients were assessed as being at the risk of malnutrition. They showed more than 7% weight loss compared to their usual body weight and poor oral intake; energy intake was less than 100% of Basal Energy Expenditure (BEE) and protein intake was less than or equal to 0.77 g/kg/d. However, only 6.3% of breast cancer patients had risk of malnutrition and their oral intake was better; energy intake was 121% of BEE, and protein intake was 0.90 g/kg/d. Outpatients receiving chemotherapy had different nutritional risk depending on their cancer site. Nutritional management program should be conducted differently, depending on the cancer site and upper gastrointestinal cancer patients at high risk of malnutrition should basically have nutritional assessment and intervention.
|