Articles
- Page Path
- HOME > Korean J Community Nutr > Volume 21(6); 2016 > Article
-
Research Article
- Dietary Changes After Breast Cancer Diagnosis: Associations with Physical Activity, Anthropometry, and Health-related Quality of life Among Korean Breast Cancer Survivors
-
Sihan Song, Hyun Jo Youn, So-Youn Jung, Eunsook Lee, Zisun Kim, Jihyoung Cho, Young Bum Yoo, Hyeong-Gon Moon, Dong-Young Noh, Jung Eun Lee

-
Korean Journal of Community Nutrition 2016;21(6):533-544.
DOI: https://doi.org/10.5720/kjcn.2016.21.6.533
Published online: December 31, 2016
1Department of Food and Nutrition, College of Human Ecology, Sookmyung Women's University, Seoul, Korea.
2Department of Surgery, Chonbuk National University Medical School, Jeonju, Korea.
3Center for Breast Cancer, National Cancer Center, Goyang, Korea.
4Department of Surgery, Soonchunhyang University College of Medicine, Bucheon, Korea.
5Department of Surgery, Keimyung University School of Medicine, Daegu, Korea.
6Department of Surgery, Konkuk University School of Medicine, Seoul, Korea.
7Breast Care Center, Seoul National University Hospital, Seoul, Korea.
8Department of Surgery and Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
9Department of Food and Nutrition, College of Human Ecology, Seoul National University, Seoul, Korea.
- Corresponding author: Jung Eun Lee. Department of Food and Nutrition, Seoul National University, College of Human Ecology, 1 Gwanak-ro, Gwanak-gu, Seoul 08826, Korea. Tel: (02) 880-6834, Fax: (02) 880-0305, jungelee@snu.ac.kr
Copyright © 2016 The Korean Society of Community Nutrition
This is an Open-Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,417 Views
- 1 Download
- 4 Crossref
Abstract
-
Objectives
- We aimed to examine levels of physical activity, anthropometric features, and health-related quality of life (HRQoL) among Korean breast cancer survivors who reported changes in their diet after diagnosis.
-
Methods
- A total of 380 women who had been diagnosed with stage I to III breast cancer and had breast cancer surgery at least six months before the interview were included. Participants provided information on dietary change after diagnosis, post-diagnostic diet, physical activity, anthropometric measures, and HRQoL through face-to-face interview. We assessed HRQoL levels of breast cancer survivors using a validated Korean version of European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ-C30) and Breast Cancer Module (BR23). We used the logistic regression and generalized linear models to identify the associations of dietary changes in relation with physical activity, anthropometry, and HRQoL.
-
Results
- The majority of participants (72.6%) reported that they have changed their diet to a healthier diet after diagnosis. Breast cancer survivors who reported to have change to a healthy diet had higher intakes of vegetables and fruits and lower intakes of red and processed meats, and refined grains than those who did not. Also, survivors with a healthy change in their diet were more likely to engage in physical activity (top vs. bottom tertile: odds ratio [OR], 1.85; 95% confidence interval [95% CI], 1.02-3.36) and have lower body mass index (BMI) (OR, 0.90; 95% CI, 0.82-0.98 for one kg/m2 increment in BMI) compared to those who did not. We found that a healthy change in diet was associated with higher scores of physical functioning (p=0.02) and lower scores of constipation (p=0.04) and diarrhea (p=0.006) compared to those who did not.
-
Conclusions
- Healthy changes in diet after breast cancer diagnosis may be associated with lower levels of BMI, and higher levels of physical activity and HRQoL.
Acknowledgments
Acknowledgments
- 1. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015; 136(5): E359-E386.ArticlePubMed
- 2. Oh CM, Won YJ, Jung KW, Kong HJ, Cho H, Lee JK. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2013. Cancer Res Treat 2016; 48(2): 436-450.ArticlePubMedPMCPDF
- 3. Kelsey JL, Gammon MD, John EM. Reproductive factors and breast cancer. Epidemiol Rev 1993; 15(1): 36-47.ArticlePubMed
- 4. Anderson KN, Schwab RB, Martinez ME. Reproductive risk factors and breast cancer subtypes: a review of the literature. Breast Cancer Res Treat 2014; 144(1): 1-10.ArticlePubMedPMCPDF
- 5. Okasha M, McCarron P, Gunnell D, Smith GD. Exposures in childhood, adolescence and early adulthood and breast cancer risk: a systematic review of the literature. Breast Cancer Res Treat 2003; 78(2): 223-276.ArticlePubMed
- 6. Turner LB. A meta-analysis of fat intake, reproduction, and breast cancer risk: an evolutionary perspective. Am J Hum Biol 2011; 23(5): 601-608.ArticlePubMed
- 7. Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 2005; 353(17): 1784-1792.ArticlePubMed
- 8. Demark-Wahnefried W, Aziz NM, Rowland JH, Pinto BM. Riding the crest of the teachable moment: promoting long-term health after the diagnosis of cancer. J Clin Oncol 2005; 23(24): 5814-5830.ArticlePubMed
- 9. Stewart DE, Cheung AM, Duff S, Wong F, McQuestion M, Cheng T. Attributions of cause and recurrence in long-term breast cancer survivors. Psychooncology 2001; 10(2): 179-183.ArticlePubMed
- 10. Rabin C, Pinto B. Cancer-related beliefs and health behavior change among breast cancer survivors and their first-degree relatives. Psychooncology 2006; 15(8): 701-712.ArticlePubMed
- 11. Costanzo ES, Lutgendorf SK, Roeder SL. Common-sense beliefs about cancer and health practices among women completing treatment for breast cancer. Psychooncology 2011; 20(1): 53-61.ArticlePubMedPMCLink
- 12. Salminen EK, Lagstrom HK, Heikkila S, Salminen S. Does breast cancer change patients' dietary habits? Eur J Clin Nutr 2000; 54(11): 844-848.ArticlePubMedPDF
- 13. Maunsell E, Drolet M, Brisson J, Robert J, Deschenes L. Dietary change after breast cancer: extent, predictors, and relation with psychological distress. J Clin Oncol 2002; 20(4): 1017-1025.ArticlePubMed
- 14. Thomson CA, Flatt SW, Rock CL, Ritenbaugh C, Newman V, Pierce JP. Increased fruit, vegetable and fiber intake and lower fat intake reported among women previously treated for invasive breast cancer. J Am Diet Assoc 2002; 102(6): 801-808.ArticlePubMed
- 15. Salminen E, Bishop M, Poussa T, Drummond R, Salminen S. Dietary attitudes and changes as well as use of supplements and complementary therapies by Australian and Finnish women following the diagnosis of breast cancer. Eur J Clin Nutr 2004; 58(1): 137-144.ArticlePubMedPDF
- 16. Vance V, Campbell S, McCargar L, Mourtzakis M, Hanning R. Dietary changes and food intake in the first year after breast cancer treatment. Appl Physiol Nutr Metab 2014; 39(6): 707-714.ArticlePubMed
- 17. Velentzis LS, Keshtgar MR, Woodside JV, Leathem AJ, Titcomb A, Perkins KA. Significant changes in dietary intake and supplement use after breast cancer diagnosis in a UK multicentre study. Breast Cancer Res Treat 2011; 128(2): 473-482.ArticlePubMedPDF
- 18. Wayne SJ, Lopez ST, Butler LM, Baumgartner KB, Baumgartner RN, Ballard-Barbash R. Changes in dietary intake after diagnosis of breast cancer. J Am Diet Assoc 2004; 104(10): 1561-1568.ArticlePubMed
- 19. Skeie G, Hjartaker A, Braaten T, Lund E. Dietary change among breast and colorectal cancer survivors and cancer-free women in the Norwegian women and cancer cohort study. Cancer Causes Control 2009; 20(10): 1955-1966.ArticlePubMedPDF
- 20. World Cancer Research Fund. American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Washington DC: AICR; 2007.
- 21. Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin 2012; 62(4): 243-274.ArticlePubMed
- 22. Patterson RE, Cadmus LA, Emond JA, Pierce JP. Physical activity, diet, adiposity and female breast cancer prognosis: a review of the epidemiologic literature. Maturitas 2010; 66(1): 5-15.ArticlePubMed
- 23. Davies NJ, Batehup L, Thomas R. The role of diet and physical activity in breast, colorectal, and prostate cancer survivorship: a review of the literature. Br J Cancer 2011; 105: Suppl 1. S52-S73.ArticlePubMedPMCPDF
- 24. Rock CL, Demark-Wahnefried W. Nutrition and survival after the diagnosis of breast cancer: a review of the evidence. J Clin Oncol 2002; 20(15): 3302-3316.ArticlePubMed
- 25. Montazeri A. Health-related quality of life in breast cancer patients: a bibliographic review of the literature from 1974 to 2007. J Exp Clin Cancer Res 2008; 27(1): 32.ArticlePubMedPMCPDF
- 26. American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2016-2017. Atlanta: American Cancer Society; 2016.
- 27. Shin DW, Cho B, Kim SY, Jung JH, Park JH. Management of cancer survivors in clinical and public health perspectives: current status and future challenges in Korea. J Korean Med Sci 2013; 28(5): 651-657.ArticlePubMedPMCLink
- 28. Song S, Hwang E, Moon HG, Noh DY, Lee JE. Adherence to guidelines for cancer survivors and health-related quality of life among Korean breast cancer survivors. Nutrients 2015; 7(12): 10307-10319.ArticlePubMedPMC
- 29. Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, et al. 2011 compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 2011; 43(8): 1575-1581.PubMed
- 30. Yun YH, Park YS, Lee ES, Bang SM, Heo DS, Park SY. Validation of the Korean version of the EORTC QLQ-C30. Qual Life Res 2004; 13(4): 863-868.ArticlePubMed
- 31. Yun YH, Bae SH, Kang IO, Shin KH, Lee R, Kwon SI. Cross-cultural application of the Korean version of the European Organization for Research and Treatment of Cancer (EORTC) Breast-Cancer-Specific Quality of Life Questionnaire (EORTC QLQ-BR23). Support Care Cancer 2004; 12(6): 441-445.ArticlePubMedPDF
- 32. Aaronson NK AS, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A. The European organization for research and treatment of cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993; 85(5): 365-376.ArticlePubMed
- 33. Schmid D, Leitzmann MF. Association between physical activity and mortality among breast cancer and colorectal cancer survivors: a systematic review and meta-analysis. Ann Oncol 2014; 25(7): 1293-1311.ArticlePubMed
- 34. Ibrahim EM, Al-Homaidh A. Physical activity and survival after breast cancer diagnosis: meta-analysis of published studies. Med Oncol 2011; 28(3): 753-765.ArticlePubMedPDF
- 35. Irwin ML, McTiernan A, Baumgartner RN, Baumgartner KB, Bernstein L, Gilliland FD. Changes in body fat and weight after a breast cancer diagnosis: influence of demographic, prognostic, and lifestyle factors. J Clin Oncol 2005; 23(4): 774-782.ArticlePubMed
- 36. Saquib N, Flatt SW, Natarajan L, Thomson CA, Bardwell WA, Caan B. Weight gain and recovery of pre-cancer weight after breast cancer treatments: evidence from the women's healthy eating and living (WHEL) study. Breast Cancer Res Treat 2007; 105(2): 177-186.ArticlePubMedPDF
- 37. Vance V, Mourtzakis M, McCargar L, Hanning R. Weight gain in breast cancer survivors: prevalence, pattern and health consequences. Obes Rev 2011; 12(4): 282-294.ArticlePubMed
- 38. Playdon MC, Bracken MB, Sanft TB, Ligibel JA, Harrigan M, Irwin ML. Weight gain after breast cancer diagnosis and all-cause mortality: Systematic review and meta-analysis. J Natl Cancer Inst 2015; 107(12): djv275.ArticlePubMedPMC
- 39. de Waard F, Ramlau R, Mulders Y, de Vries T, van Waveren S. A feasibility study on weight reduction in obese postmenopausal breast cancer patients. Eur J Cancer Prev 1993; 2(3): 233-238.ArticlePubMed
- 40. Hebert JR, Ebbeling CB, Olendzki BC, Hurley TG, Ma Y, Saal N. Change in women's diet and body mass following intensive intervention for early-stage breast cancer. J Am Diet Assoc 2001; 101(4): 421-431.ArticlePubMed
- 41. Buzzard IM, Asp EH, Chlebowski RT, Boyar AP, Jeffery RW, Nixon DW. Diet intervention methods to reduce fat intake: nutrient and food group composition of self-selected low-fat diets. J Am Diet Assoc 1990; 90(1): 42-50. 53.ArticlePubMed
- 42. Wayne SJ, Baumgartner K, Baumgartner RN, Bernstein L, Bowen DJ, Ballard-Barbash R. Diet quality is directly associated with quality of life in breast cancer survivors. Breast Cancer Res Treat 2006; 96(3): 227-232.ArticlePubMedPDF
- 43. Blanchard CM, Courneya KS, Stein K. Cancer survivors' adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American cancer society's SCS-II. J Clin Oncol 2008; 26(13): 2198-2204.ArticlePubMed
- 44. Inoue-Choi M, Lazovich D, Prizment AE, Robien K. Adherence to the World Cancer Research Fund/American Institute for Cancer Research recommendations for cancer prevention is associated with better health-related quality of life among elderly female cancer survivors. J Clin Oncol 2013; 31(14): 1758-1766.ArticlePubMedPMC
- 45. Song S, Youn J, Park M, Hwang E, Moon HG, Noh DY, et al. The association between the adherence to dietary guidelines for breast cancer survivors and health-related quality of life among Korean breast cancer survivors. Korean J Community Nutr 2015; 20(2): 129-140.Article
REFERENCES
Demographic, clinical and lifestyle characteristics of study participants according to change to a healthy diet after diagnosis of breast cancer
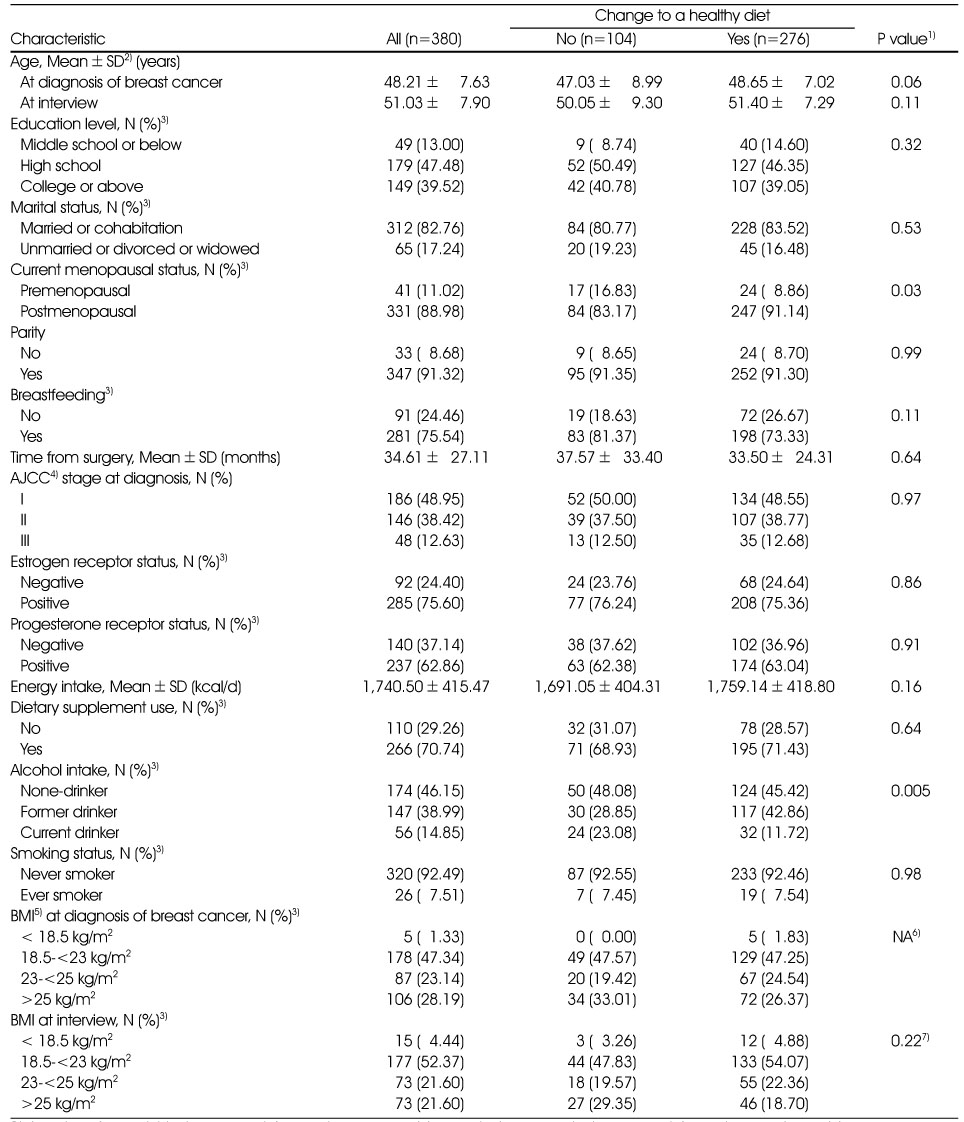
1) Log transformed t-test was used for continuous variables and chi-square test was used for categorical variables.
2) SD: standard deviation
3) Number of participants did not equal to 380 because some participants did not provide the relevent information.
4) AJCC: American Joint Committee on Cancer
5) BMI: body mass index
6) NA: Not available
7) Fisher exact test was used.
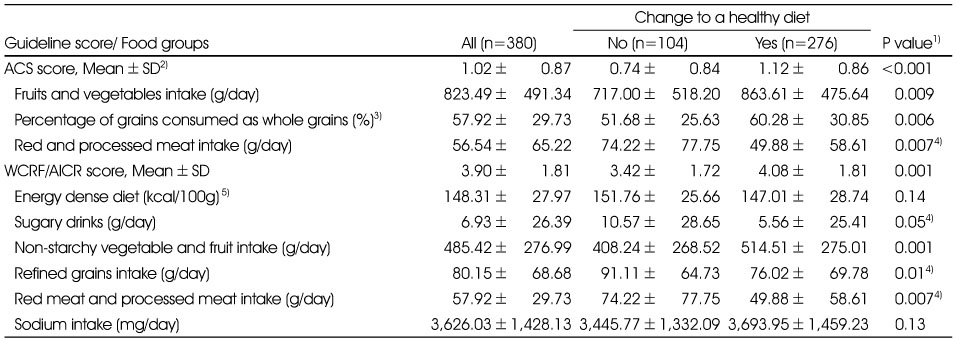
Adherence score of American Cancer Society (ACS) or World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) guidelines and intake of food groups at interview according to change to a healthy diet after diagnosis of breast cancer (n=380)
Odds ratio (OR) and 95% confidence interval (CI) for change to a healthy diet by physical activity and anthropometric measures (n=380)
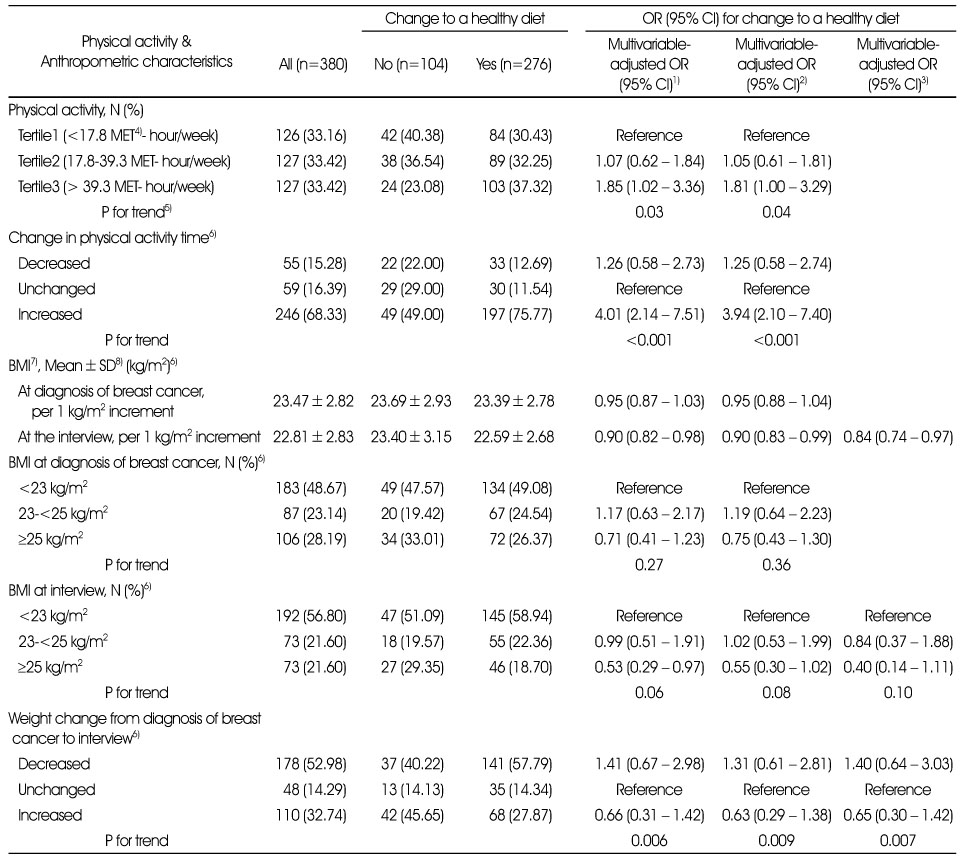
1) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), stage of breast cancer (I, II, III), and alcohol intake (never, former, current).
2) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), stage of breast cancer (I, II, III), and alcohol intake (never, former, current). For physical activity, BMI at diagnosis (<23, 23-<25, ≥25 kg/m2) was additionally adjusted. For BMI or weight change, physical activity (MET hours/week, tertile) was additionally adjusted.
3) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), stage of breast cancer (I, II, III), and alcohol intake (never, former, current), physical activity (MET hours/week, tertile), and BMI at diagnosis (<23, 23-<25, ≥25 kg/m2).
4) MET: metabolic equivalent task.
5) P for trend was calculated by assigning median or ordinal value as continuous variable.
6) Number of participants did not equal to 380 because some participants did not provide the relevant information.
7) BMI: body mass index
8) SD: standard deviation
Health-related quality of life (HRQoL) scores according to change to a healthy diet after diagnosis of breast cancer (n=204)
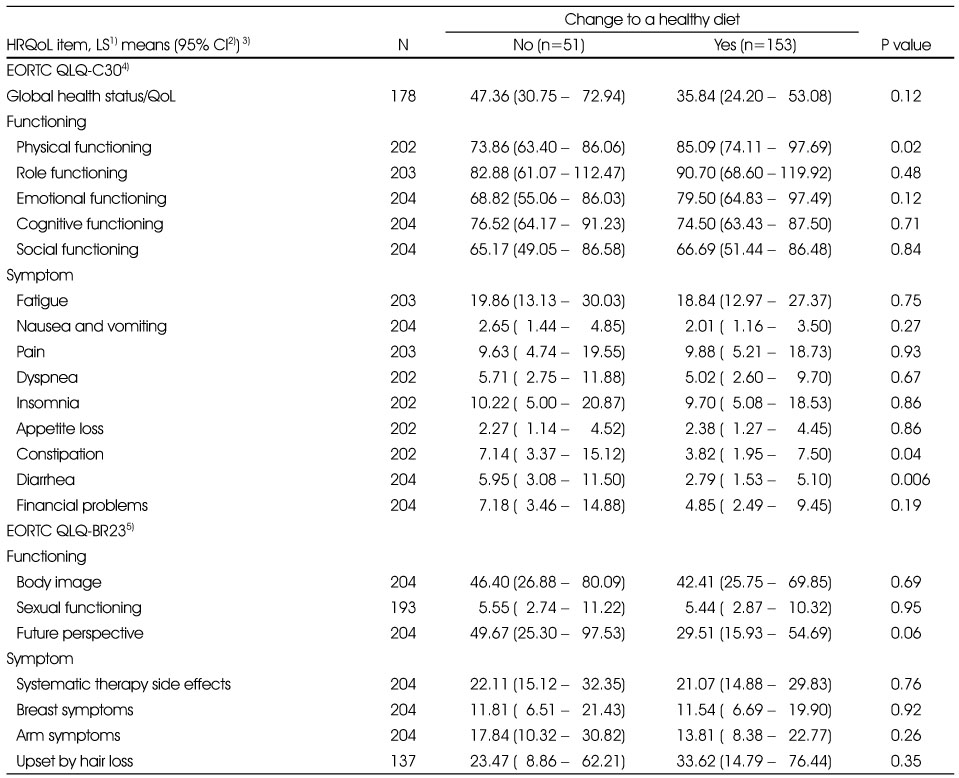
1) LS means: least-squares means
2) 95% CI: 95% confidence interval
3) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), body mass index at diagnosis (<23, 23-<25, ≥25 kg/m2), marital status (married or cohabitation, unmarried or divorced or widowed), current menopausal status (premenopausal, postmenopausal), education level (middle school or below, high school, and college or above), stage of breast cancer (I, II, III), time from breast cancer surgery (6 month-<1 year, 1 year-<5 years, ≥5 years), and alcohol intake (never, former, current).
4) EORTC QLQ-30: EUROPEAN Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30
5) BR23: breast cancer module
Figure & Data
REFERENCES
Citations

- Development and Effects of a Smartphone Application to Improve Self-Management in Workers Who Underwent Thyroid Cancer Surgery
Myoyoun Kim, Seon Young Hwang
Cancer Nursing.2025;[Epub] CrossRef - Health-Related Behaviors of Middle-Aged Cancer Survivors: A Comparative Study with Matched Non-Cancer Controls Using the Korea National Health and Nutrition Examination Survey VI–VII (2013–2018) Data
Mi Lee KIM, Ju Ri JEONG, Yu Ri CHOE
Korean Journal of Health Promotion.2025; 25(1): 20. CrossRef - Cancer survivor's dietary safety management awareness and competency type
Yun Hwa Kim
Journal of Nutrition and Health.2020; 53(5): 532. CrossRef - Health-related Quality of Life and Its Related Factors among Cancer Survivors and General Adults: Focusing on Lifestyle Behaviors and Mental Health
Eun A Song, Youngran Kweon, Yoon Young Hwang, Minjeong An
Korean Journal of Adult Nursing.2020; 32(4): 385. CrossRef
Demographic, clinical and lifestyle characteristics of study participants according to change to a healthy diet after diagnosis of breast cancer
1) Log transformed t-test was used for continuous variables and chi-square test was used for categorical variables.
2) SD: standard deviation
3) Number of participants did not equal to 380 because some participants did not provide the relevent information.
4) AJCC: American Joint Committee on Cancer
5) BMI: body mass index
6) NA: Not available
7) Fisher exact test was used.
Adherence score of American Cancer Society (ACS) or World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) guidelines and intake of food groups at interview according to change to a healthy diet after diagnosis of breast cancer (n=380)
1) T-test was used for comparing two groups.
2) SD: standard deviation
3) Among 380, one participant was excluded.
4) Wilcoxon-Mann-Whitney test was used for comparing two groups.
5) Energy dense diet denotes energy intake per amount of total food intake (kcal per 100 g).
Odds ratio (OR) and 95% confidence interval (CI) for change to a healthy diet by physical activity and anthropometric measures (n=380)
1) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), stage of breast cancer (I, II, III), and alcohol intake (never, former, current).
2) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), stage of breast cancer (I, II, III), and alcohol intake (never, former, current). For physical activity, BMI at diagnosis (<23, 23-<25, ≥25 kg/m2) was additionally adjusted. For BMI or weight change, physical activity (MET hours/week, tertile) was additionally adjusted.
3) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), stage of breast cancer (I, II, III), and alcohol intake (never, former, current), physical activity (MET hours/week, tertile), and BMI at diagnosis (<23, 23-<25, ≥25 kg/m2).
4) MET: metabolic equivalent task.
5) P for trend was calculated by assigning median or ordinal value as continuous variable.
6) Number of participants did not equal to 380 because some participants did not provide the relevant information.
7) BMI: body mass index
8) SD: standard deviation
Health-related quality of life (HRQoL) scores according to change to a healthy diet after diagnosis of breast cancer (n=204)
1) LS means: least-squares means
2) 95% CI: 95% confidence interval
3) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), body mass index at diagnosis (<23, 23-<25, ≥25 kg/m2), marital status (married or cohabitation, unmarried or divorced or widowed), current menopausal status (premenopausal, postmenopausal), education level (middle school or below, high school, and college or above), stage of breast cancer (I, II, III), time from breast cancer surgery (6 month-<1 year, 1 year-<5 years, ≥5 years), and alcohol intake (never, former, current).
4) EORTC QLQ-30: EUROPEAN Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30
5) BR23: breast cancer module
1) Log transformed t-test was used for continuous variables and chi-square test was used for categorical variables. 2) SD: standard deviation 3) Number of participants did not equal to 380 because some participants did not provide the relevent information. 4) AJCC: American Joint Committee on Cancer 5) BMI: body mass index 6) NA: Not available 7) Fisher exact test was used.
1) T-test was used for comparing two groups. 2) SD: standard deviation 3) Among 380, one participant was excluded. 4) Wilcoxon-Mann-Whitney test was used for comparing two groups. 5) Energy dense diet denotes energy intake per amount of total food intake (kcal per 100 g).
1) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), stage of breast cancer (I, II, III), and alcohol intake (never, former, current). 2) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), stage of breast cancer (I, II, III), and alcohol intake (never, former, current). For physical activity, BMI at diagnosis (<23, 23-<25, ≥25 kg/m2) was additionally adjusted. For BMI or weight change, physical activity (MET hours/week, tertile) was additionally adjusted. 3) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), stage of breast cancer (I, II, III), and alcohol intake (never, former, current), physical activity (MET hours/week, tertile), and BMI at diagnosis (<23, 23-<25, ≥25 kg/m2). 4) MET: metabolic equivalent task. 5) P for trend was calculated by assigning median or ordinal value as continuous variable. 6) Number of participants did not equal to 380 because some participants did not provide the relevant information. 7) BMI: body mass index 8) SD: standard deviation
1) LS means: least-squares means 2) 95% CI: 95% confidence interval 3) Models were adjusted for age (year; continuous), energy intake (kcal/day; continuous), body mass index at diagnosis (<23, 23-<25, ≥25 kg/m2), marital status (married or cohabitation, unmarried or divorced or widowed), current menopausal status (premenopausal, postmenopausal), education level (middle school or below, high school, and college or above), stage of breast cancer (I, II, III), time from breast cancer surgery (6 month-<1 year, 1 year-<5 years, ≥5 years), and alcohol intake (never, former, current). 4) EORTC QLQ-30: EUROPEAN Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 5) BR23: breast cancer module

 KSCN
KSCN
 Cite
Cite


