Articles
- Page Path
- HOME > Korean J Community Nutr > Volume 18(4); 2013 > Article
-
Original Article
- Effectiveness of Nutrition Education and Counseling on the Salty Taste Assessment, Nutrition Knowledge and Dietary Attitude of Hemodialysis Patients
- Young-Mi Lee, Yeon-Kyung Lee
-
Korean Journal of Community Nutrition 2013;18(4):402-412.
DOI: https://doi.org/10.5720/kjcn.2013.18.4.402
Published online: August 31, 2013
Nutrition Education Major, Graduate School of Education, Kyungpook National University, Daegu, Korea.
1Department of Food Science and Nutrition, Kyungpook National University, Daegu, Korea.
- Corresponding author: Yeon-Kyung Lee, Department of Food Science and Nutrition, Kyungpook National University, 1370 Sankyuk Dong, Buk-ku, Daegu 702-201, Korea. Tel: (053) 950-6234, Fax: (053) 950-6229, yklee@knu.ac.kr
Copyright © 2013 The Korean Society of Community Nutrition
This is an Open-Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,210 Views
- 6 Download
- 2 Crossref
Abstract
- The purpose of this study was to evaluate the effectiveness of nutrition education and counseling on the salty taste assessment, nutrition knowledge and dietary attitude of 21 hemodialysis patients. Five times of the nutrition education and three times of nutrition counseling were performed for a period of 5 months. Biochemical analysis revealed that creatinine was significantly high (p < 0.001), blood urea nitrogen and serum albumin were significantly low (p < 0.05, p < 0.01) and Na, K, Cl, K, P and uric acid were not significantly different. The distribution rate of unsalty taste preference were significantly high and the distribution rate of salty taste preference were significantly low after nutrition education and counseling (p < 0.001). Nutrition knowledge significantly improved following 5th month of education and counseling (p < 0.01). Particularly, the scores for questions related to sodium were improved. The dietary attitude was significantly improved during the counseling period (p < 0.05). There were improvements in responses to 'use food exchange list on diet' and 'habitually add salt or soy sauce before the meal'. According to these results, salty taste assessment, nutrition knowledge and dietary attitude were significantly improved by the hemodialysis diet therapy practices of hemodialysis patients. Therefore, we conclude that there was a need for low-salt diet education and nutrition counseling to help them recognize the taste of low-salt foods and strive towards a preference for less salty tasting foods and the consumption of a low-salt diet.
- 1. Cho YH, Yoon JB, Kim SR. Effect of hemodialysis on taste acuity in patient with end-stage renal disease. Korean J Nephrol 1999; 18(2): 307-312.
- 2. Cho YW, Kim GB. The present status of nutrition education in medical area - centered on the status of Korea. Proceedings of 1989 fall conference of the Korean Nutrition Society. 1998; p. 52-56.
- 3. Guthrie HA, Crocetti AF. Variability of nutrition intake over a 3-day peroid. J Am Diet Assoc 1985; 85(3): 325-327.PubMed
- 4. Han DS. Dietetic theraphy of chronic renal failure. Korean J Intern Med 1989; 37(1): 1-10.
- 5. Jang YG, Byeon GW, Lee BG, Lee JH, Lee HM, Jo YY. Medical nutrition therapy. Seoul: Hyoil; 2006. p. 341-355.
- 6. Jeon SY, Kang GY, YU MH. Diet therapy. Seoul: Gwanmungak; 1993. p. 235-256.
- 7. Jung HJ. Effect of nutrition education and counseling on dietary therapy action in type diabetes patients. Kyungpook National University; 2011; 42. 61-62 MS thesis.
- 8. Kang SS. Effect of pre-dialysis nutrition education on nutritional status of hemodialysis patients. Ewha womens University; 2003; MS thesis.
- 9. Kim HH, Shin EK, Lee HJ, Lee NH, Chun BY, Ahn MY, Lee YK. Evaluation of the effectiveness of a salt reduction program for employees. Korean J Nutr 2009; 42(4): 350-357.Article
- 10. Kim HJ, Kim SA, Sohn CM. Association of the nutritional status and essential amino acids intake in hemodialysis patients. Korean J Nutr 2006; 39(7): 617-623.
- 11. Kim JY, Kwon KH, Choi HY, Kim KS, Yang YK. Comparison of nutritional status according to serum C-reactive protein concentration in hemodialysis patients. Korean J Nephrol 2000a; 19(3): 461-467.
- 12. Kim SM, Lee YS, Cho DK. Nutritional assessment of the hemodialysis patients. Korean J Nutr 2000b; 33(2): 179-185.
- 13. Kim , YH , Seo HJ, Kim SR. A study of the nutritional status, nutritional knowledge, and dietary habits of the hemodialysis patients. Korean J Nutr 2001; 34(8): 920-928.
- 14. Kopple JD. Abnormal amino acid and protein metabolism in uremia. Kidney Int 1978; 14(4): 340-348.ArticlePubMed
- 15. Kopple JD. Nutrition, Diet and the Kidney. 7th Ed. Philadelphia: 1988. p. 1230-1286.
- 16. Kopple JD. Protein-energy malnutrition in maintenance dialysis patients. Am J Clin Nutr 1997; 65(5): 1544-1577.PubMed
- 17. Kopple JD, Jones M, Fukuda S, Swendseid ME. Amino acid and protein metabolism in renal failure. Am J Clin Nutr 1978; 31(9): 1532-1540.ArticlePubMed
- 18. Korea Health Industry Development Institute. National food & nutrition statistics: based on 2010 Korea National Health and Nutrition Examination Survey. 2012.
- 19. Lee HT, Cho S, Lee SH, Kim SR, Kim YH, Seo HJ. Influence of routine calorie and protein intake on nutritional status in stable chronic hemodialysis patients : A 18 months follow-up study. Korean J Nephrol 2002; 21(1): 129-136.
- 20. Lee HW. Healthy living dialysis. Seoul: Jungmyeong; 2004.
- 21. Lee JH, Ahn SH, Song JH. Factors influencing malnutrition in maintenance hemodialysis patients. Korean J Nephrol 2000; 19(5): 778-783.
- 22. Lee NY, Jang YG, Park HC. The research on the nutritional status of hemodialysis patients and nutrition knowledge. Proceedings of 2004 fall Conference of the Korean Society of Community Nutrition (Poster Presentation); 2004; p. 423.
- 23. Min HS, Lee EJ. A study of relationship between compliance with therapeutic regimens and physiological parameters of hemodialysis patients. J Korean Acad Nurs 2006; 36(1): 64-73.ArticlePDF
- 24. Schoenfeld PY, Henry RR, Laird NM, Roxe DM. Assessment of nutritional status of the national cooperative dailysis study population. Kidney Int Suppl 1983 04; (13): S80-S88.PubMed
- 25. Shin EK, Lee HJ, Ahn MY, Lee YK. Study on the development and evaluation of validity of salty taste assessment tool. Korean J Nutr 2008a; 41(2): 184-191.
- 26. Shin EK, Lee HJ, Jun SY, Park EJ, Jung YY, Ahn MY, Lee YK. Development and evaluation of nutrition education program for sodium reduction in foodservice operation. Korean J Community Nutr 2008b; 13(2): 216-227.
- 27. The Korean Dietetic Association. Manual of medical nutrition therapy. The 3rd ed. Seoul: The Korean Dietetic Association; 2008.
- 28. The Korean Society Nephrology. Current renal replacement therapy in Korea. Insan mimorial dialysis registry, 2009. ESRD Registry Committee, Korea Society of Nephrology; 2009; cited 2011 April 30]. Available from http://www.ksn.or.kr/journal/2010/index.html.
- 29. Thunberg BJ, Swamy AC, Cestero RV. Cross-sectional and longitudinal nutritional measurements in maintenance hemodialysis patients. Am J Clin Nutr 1981; 34(10): 2005-2012.ArticlePubMed
- 30. Walser M. Nutrition in renal failure. Annu Rev Nutr 1983; 3: 125-154.ArticlePubMed
- 31. Yang JL, Seo HJ, Kim YH. Effects of nutrition educational status of hemodialysis patients. Korean J Nutr 2003; 36(7): 749-758.
- 32. Youn DJ, Kim JK, Choi SJ, Choi TY, Hwang SD. Nutritional status and plasma amino acid profile in maintenance hemodialysis patients. Korean J Med 2002; 62(5): 522-529.
- 33. Young GA, Dibble JB, Hobson SM, Tompkins L, Gibson J, Turney JH, Brownjohn AM. The use of an amino-acid-based CAPD fluid over 12 weeks. Nephrol Dial Transplant 1989; 4(4): 285-292.ArticlePubMed
- 34. Young GA, Kopple JD, Lindholm B, Vonesh EF, De Vecchi A, Scalamogna A, Castelnova C, Oreopoulos DG, Anderaon GH, Bergstorm J, Dichiro J, Prowant BF, Algrim CE, Martis L, Serkes KD. Nutritional assessment of continuous ambulatory peritoneal dialysis patients : an international study. Am J Kidney Dis 1991; 17(4): 462-471.ArticlePubMed
- 35. Yu JA, Lee YW, Kim JG. A study on the perception of salt and food intake of hemodialysis patients. J Korean Public Helath Assoc 2000; 26(1): 104-115.
REFERENCES
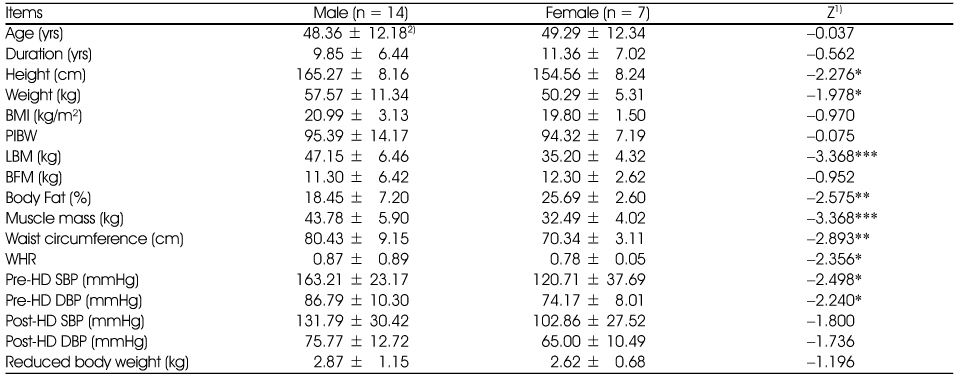
1) Z-value by Mann-Whitney Test
2) Mean ± SD
BMI: Body Mass Index [weight (kg)/height (m2)], PIBW: Percent Ideal Body Weight, LBM: Lean Body Mass, BFM: Body Fat Mass, %BF: Percent Body Fat, WHR: Waist-Hip circumference Ratio, Pre-HD : Pre-hemodialysis, Post-HD : Post-hemodialysis, SBP : Systolic Blood Pressure, DBP : Diastolic Blood Pressure
*:p < 0.05, **:p < 0.01, ***:p < 0.001 by Mann-Whitney Test
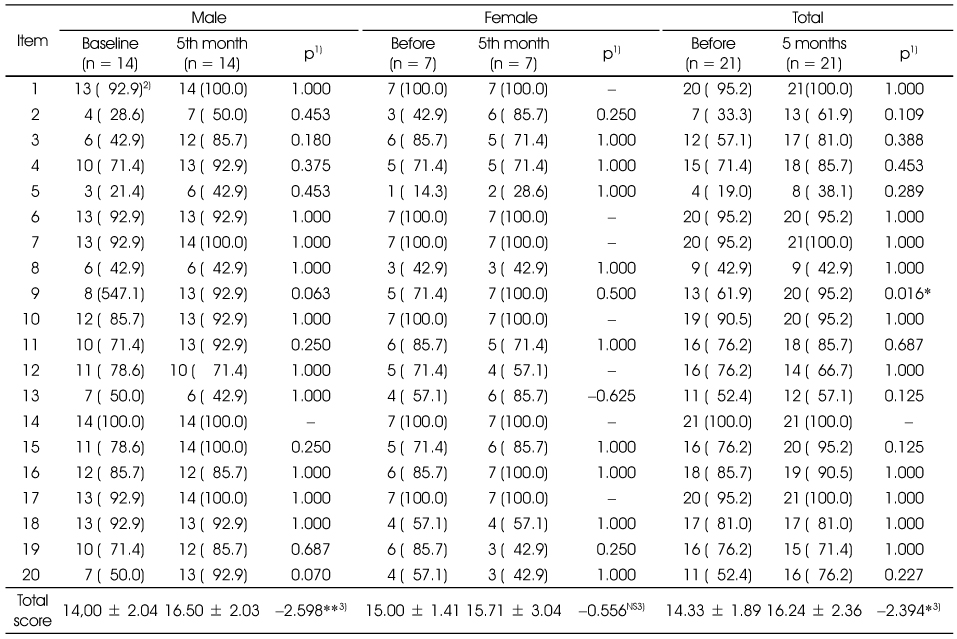
1) p-value by Mcnemar Test
2) N (%)
3) χ2-value by Wilcoxon Test
NS: Not Significant between groups by Wilcoxon Test
*:p < 0.05, **:p < 0.01
1. Of the following information, what is incorrect information for hemodialysis patients?
2. What is the correct way to supplement nutritional energy in the diets of hemodialysis patients?
3. Which high-quality protein is not good for hemodialysis patients?
4. Hemodialysis patients should limit the intake of which nutrient (s)?
5. What is the daily allowance of sodium intake for hemodialysis patients?
6. What is the daily allowance of water intake for hemodialysis patients?
7. Which food do you have to limit because of its high potassium content?
8. Which foods are rich in phosphorus and therefore, you do not need to limit their consumption?
9. What seasoning does not require limited usage?
10. What problems occur when eating out?
11. It is recommended to eat frozen or chilled fruits between meals because it is a good way to relieve thirst. (O)
12. Put water in a large container so that water is available for you to drink when you are thirsty and need to drink water. (O)
13. When cooking vegetables, use stems rather than leaves or hearts. (×)
14. If you eat raw vegetables, eat them only after they have been chopped and then, rinsed several times in water. (O)
15. It is better to use the water used for blanching vegetables when you cook. (×)
16. Hemodialysis patients do not need to restrict their calorie or protein intake. (×)
17. Eat several raw vegetables such as seaweed and spinach for dietary fiber. (×)
18. Sodium, as a component of salt, is 40% of salt. (O)
19. Salt can help balance moisture content in our bodies. (O)
20. Food additives in manufactured foods such as baking powder, raising agent, and sodium bicarbonate are harmful to human health. However, food additives do not contain sodium. (×)
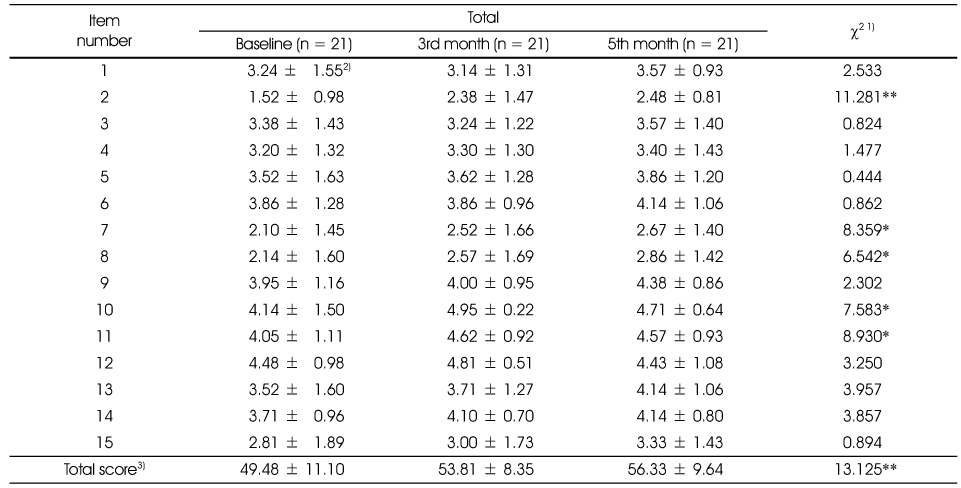
1) χ2-value by Friedman Test
2) Mean ± SD
3) Total score = 75 point, Quite agree: 5 points, Not agree at all: 1 point
*:p < 0.05, **:p < 0.01 by Friedman Test
1. I try to apply nutrition knowledge to my daily diet.
2. I apply the food exchange list to my daily diet.
3. When I prepare and/or eat a meal, I am interested in the food ingredients.
4. When I prepare and/or eat a meal, I consider nutritional balance.
5. When I eat out, I am careful of sodium, phosphorus and potassium intake.
6. I try not to overeat on holidays or when eating out.
7. When I buy processed foods, I carefully read the nutrition facts.
8. When I buy processed foods, I check the amount of sodium on nutrition labels.
9. When I cook, I try to reduce salty flavor.
10. I have the habit of adding salt or soy sauce before I eat certain foods.
11. When the food is not salty, I add more salt or soy sauce.
12. When I eat bread, I spread plenty of margarine or butter on it.
13. When I eat soup or stew, I eat a lot of soup broth.
14. I eat a lot of kimchi at every meal.
15. When I eat out, I ask them to prepare my food with less/no salt
Figure & Data
REFERENCES
Citations

- Malnutrition risk, nutritional knowledge, and dietary intake in chronic kidney disease patients on hemodialysis: comparison according to coexisting diabetes
HyunJung Yoo, Sang Cheol Lee, Hye-Kyeong Kim
Journal of Nutrition and Health.2024; 57(5): 481. CrossRef - Comparison Between Semi-Quantitative Frequency Methods and 7-day Dietary Records Methods in Food and Nutrition Intake Status For Hemodialysis Patients
Dong-Ryeol Ryu, Jung-Hyun Kim, Hyun-Jung Kim, Min-Sook Kyung, Jung-Tak Park
Korean Journal of Community Nutrition.2017; 22(5): 426. CrossRef
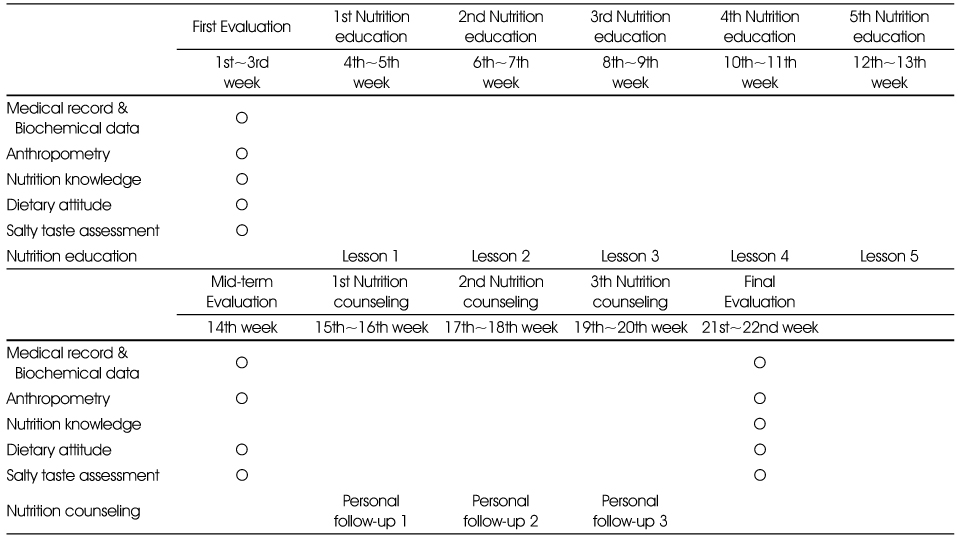
Flow chart of nutrition education and counseling
Anthropometric measurements of the subjects
1) Z-value by Mann-Whitney Test
2) Mean ± SD
BMI: Body Mass Index [weight (kg)/height (m2)], PIBW: Percent Ideal Body Weight, LBM: Lean Body Mass, BFM: Body Fat Mass, %BF: Percent Body Fat, WHR: Waist-Hip circumference Ratio, Pre-HD : Pre-hemodialysis, Post-HD : Post-hemodialysis, SBP : Systolic Blood Pressure, DBP : Diastolic Blood Pressure
*:p < 0.05, **:p < 0.01, ***:p < 0.001 by Mann-Whitney Test
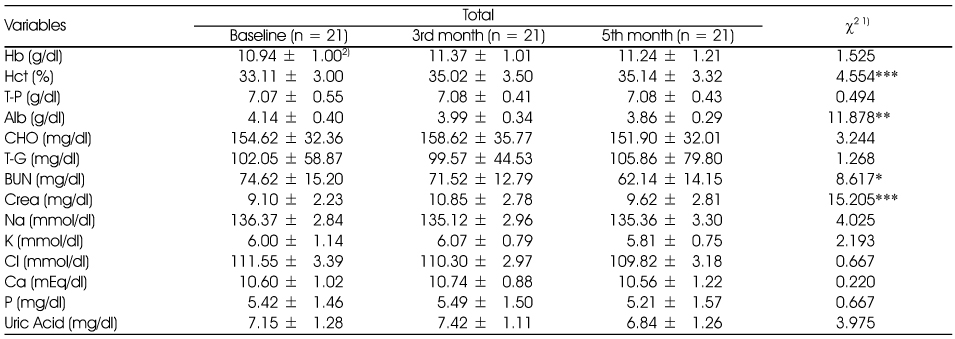
Changes in the biochemical data of the subjects after the intervention
1) χ2-value by Friedman Test
2) Mean ± SD
Hb: Hemoglobin, Hct: Hematocrit, T-P: Total protein, Alb: Albumin, CHO: Total cholesterol, T-G: Triglyceride, BUN: Blood urea nitrogen, Crea: Creatinine
*p < 0.05, **:p < 0.01, ***: p < 0.001 by Friedman Test
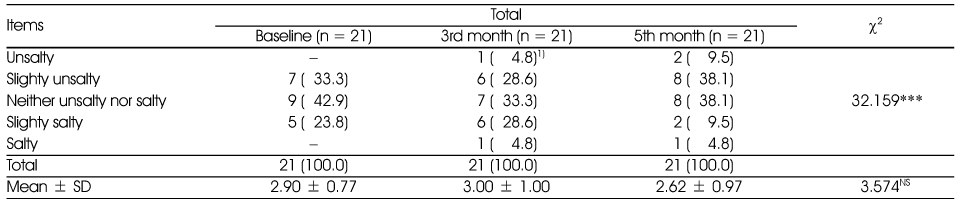
Changes in salty taste assessment of the subjects before and after counseling
1) N (%)
NS: Not Significant among 3 periods by Friedman Test
***:p < 0.001 by chi-square Test
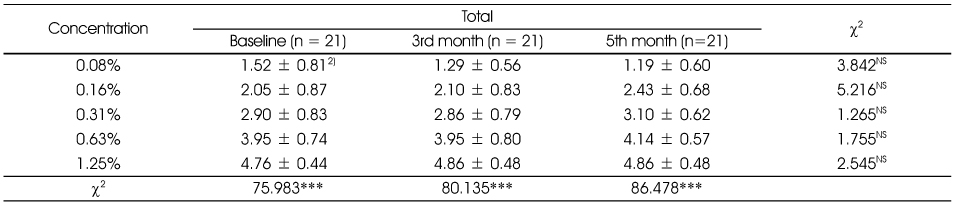
Comparison of the intensity1) by salt concentration
1) Unsalty; 1, slighty unsalty; 2, neither unsalty nor salty; 3, slighty salty; 4, salty; 5
2) Mean ± SD
NS: Not Significant among 3 periods by Friedman Test
***:p < 0.001 by Kruskal-Wallis Test
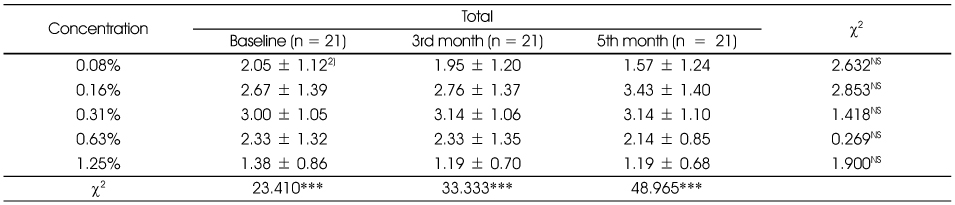
Comparison of the preference1) for salty taste during counseling
1) Dislike: 1 point, Like: 5 points
2) Mean ± SD
NS: Not Significant among 3 periods by Friedman Test
***:p < 0.001 by Kruskal-Wallis Test
Nutrition knowledge of the subjects before and after counseling
1) p-value by Mcnemar Test
2) N (%)
3) χ2-value by Wilcoxon Test
NS: Not Significant between groups by Wilcoxon Test
*:p < 0.05, **:p < 0.01
1. Of the following information, what is incorrect information for hemodialysis patients?
2. What is the correct way to supplement nutritional energy in the diets of hemodialysis patients?
3. Which high-quality protein is not good for hemodialysis patients?
4. Hemodialysis patients should limit the intake of which nutrient (s)?
5. What is the daily allowance of sodium intake for hemodialysis patients?
6. What is the daily allowance of water intake for hemodialysis patients?
7. Which food do you have to limit because of its high potassium content?
8. Which foods are rich in phosphorus and therefore, you do not need to limit their consumption?
9. What seasoning does not require limited usage?
10. What problems occur when eating out?
11. It is recommended to eat frozen or chilled fruits between meals because it is a good way to relieve thirst. (O)
12. Put water in a large container so that water is available for you to drink when you are thirsty and need to drink water. (O)
13. When cooking vegetables, use stems rather than leaves or hearts. (×)
14. If you eat raw vegetables, eat them only after they have been chopped and then, rinsed several times in water. (O)
15. It is better to use the water used for blanching vegetables when you cook. (×)
16. Hemodialysis patients do not need to restrict their calorie or protein intake. (×)
17. Eat several raw vegetables such as seaweed and spinach for dietary fiber. (×)
18. Sodium, as a component of salt, is 40% of salt. (O)
19. Salt can help balance moisture content in our bodies. (O)
20. Food additives in manufactured foods such as baking powder, raising agent, and sodium bicarbonate are harmful to human health. However, food additives do not contain sodium. (×)
Comparison of dietary attitude score before and after counseling
1) χ2-value by Friedman Test
2) Mean ± SD
3) Total score = 75 point, Quite agree: 5 points, Not agree at all: 1 point
*:p < 0.05, **:p < 0.01 by Friedman Test
1. I try to apply nutrition knowledge to my daily diet.
2. I apply the food exchange list to my daily diet.
3. When I prepare and/or eat a meal, I am interested in the food ingredients.
4. When I prepare and/or eat a meal, I consider nutritional balance.
5. When I eat out, I am careful of sodium, phosphorus and potassium intake.
6. I try not to overeat on holidays or when eating out.
7. When I buy processed foods, I carefully read the nutrition facts.
8. When I buy processed foods, I check the amount of sodium on nutrition labels.
9. When I cook, I try to reduce salty flavor.
10. I have the habit of adding salt or soy sauce before I eat certain foods.
11. When the food is not salty, I add more salt or soy sauce.
12. When I eat bread, I spread plenty of margarine or butter on it.
13. When I eat soup or stew, I eat a lot of soup broth.
14. I eat a lot of kimchi at every meal.
15. When I eat out, I ask them to prepare my food with less/no salt
1) Z-value by Mann-Whitney Test 2) Mean ± SD BMI: Body Mass Index [weight (kg)/height (m2)], PIBW: Percent Ideal Body Weight, LBM: Lean Body Mass, BFM: Body Fat Mass, %BF: Percent Body Fat, WHR: Waist-Hip circumference Ratio, Pre-HD : Pre-hemodialysis, Post-HD : Post-hemodialysis, SBP : Systolic Blood Pressure, DBP : Diastolic Blood Pressure *:p < 0.05, **:p < 0.01, ***:p < 0.001 by Mann-Whitney Test
1) χ2-value by Friedman Test 2) Mean ± SD Hb: Hemoglobin, Hct: Hematocrit, T-P: Total protein, Alb: Albumin, CHO: Total cholesterol, T-G: Triglyceride, BUN: Blood urea nitrogen, Crea: Creatinine *p < 0.05, **:p < 0.01, ***: p < 0.001 by Friedman Test
1) N (%) NS: Not Significant among 3 periods by Friedman Test ***:p < 0.001 by chi-square Test
1) Unsalty; 1, slighty unsalty; 2, neither unsalty nor salty; 3, slighty salty; 4, salty; 5 2) Mean ± SD NS: Not Significant among 3 periods by Friedman Test ***:p < 0.001 by Kruskal-Wallis Test
1) Dislike: 1 point, Like: 5 points 2) Mean ± SD NS: Not Significant among 3 periods by Friedman Test ***:p < 0.001 by Kruskal-Wallis Test
1) p-value by Mcnemar Test 2) N (%) 3) χ2-value by Wilcoxon Test NS: Not Significant between groups by Wilcoxon Test *:p < 0.05, **:p < 0.01 1. Of the following information, what is incorrect information for hemodialysis patients? 2. What is the correct way to supplement nutritional energy in the diets of hemodialysis patients? 3. Which high-quality protein is not good for hemodialysis patients? 4. Hemodialysis patients should limit the intake of which nutrient (s)? 5. What is the daily allowance of sodium intake for hemodialysis patients? 6. What is the daily allowance of water intake for hemodialysis patients? 7. Which food do you have to limit because of its high potassium content? 8. Which foods are rich in phosphorus and therefore, you do not need to limit their consumption? 9. What seasoning does not require limited usage? 10. What problems occur when eating out? 11. It is recommended to eat frozen or chilled fruits between meals because it is a good way to relieve thirst. (O) 12. Put water in a large container so that water is available for you to drink when you are thirsty and need to drink water. (O) 13. When cooking vegetables, use stems rather than leaves or hearts. (×) 14. If you eat raw vegetables, eat them only after they have been chopped and then, rinsed several times in water. (O) 15. It is better to use the water used for blanching vegetables when you cook. (×) 16. Hemodialysis patients do not need to restrict their calorie or protein intake. (×) 17. Eat several raw vegetables such as seaweed and spinach for dietary fiber. (×) 18. Sodium, as a component of salt, is 40% of salt. (O) 19. Salt can help balance moisture content in our bodies. (O) 20. Food additives in manufactured foods such as baking powder, raising agent, and sodium bicarbonate are harmful to human health. However, food additives do not contain sodium. (×)
1) χ2-value by Friedman Test 2) Mean ± SD 3) Total score = 75 point, Quite agree: 5 points, Not agree at all: 1 point *:p < 0.05, **:p < 0.01 by Friedman Test 1. I try to apply nutrition knowledge to my daily diet. 2. I apply the food exchange list to my daily diet. 3. When I prepare and/or eat a meal, I am interested in the food ingredients. 4. When I prepare and/or eat a meal, I consider nutritional balance. 5. When I eat out, I am careful of sodium, phosphorus and potassium intake. 6. I try not to overeat on holidays or when eating out. 7. When I buy processed foods, I carefully read the nutrition facts. 8. When I buy processed foods, I check the amount of sodium on nutrition labels. 9. When I cook, I try to reduce salty flavor. 10. I have the habit of adding salt or soy sauce before I eat certain foods. 11. When the food is not salty, I add more salt or soy sauce. 12. When I eat bread, I spread plenty of margarine or butter on it. 13. When I eat soup or stew, I eat a lot of soup broth. 14. I eat a lot of kimchi at every meal. 15. When I eat out, I ask them to prepare my food with less/no salt

 KSCN
KSCN
 Cite
Cite


