Articles
- Page Path
- HOME > Korean J Community Nutr > Volume 28(2); 2023 > Article
- Research Article
- Effectiveness of a mobile health intervention on weight loss and dietary behavior changes among employees with overweight and obesity: a 12-week intervention study investigating the role of engagement
- Imhuei Son, Jiyoun Hong, Young-Hee Han, Bo Jeong Gong, Meng Yuan Zhang, Woori Na, Cheongmin Sohn, Taisun Hyun
-
Korean Journal of Community Nutrition 2023;28(2):141-159.
DOI: https://doi.org/10.5720/kjcn.2023.28.2.141
Published online: April 30, 2023

2Associate professor, Department of Food and Biotechnology, Korea University, Sejong, Korea

3Invited professor, Department of Food and Nutrition, Chungbuk National University, Cheongju, Korea

4Master’s graduate, Department of Food and Nutrition, Chungbuk National University, Cheongju, Korea

5Invited professor, Department of Food and Nutrition, Wonkwang University, Iksan, Korea

6Professor, Department of Food and Nutrition, Wonkwang University, Iksan, Korea

7Professor, Department of Food and Nutrition, Chungbuk National University, Cheongju, Korea

-
Corresponding author:
Taisun Hyun, Tel: +82-43-261-2790, Fax: +82-43-267-2742,
Email: taisun@cbnu.ac.kr
- 1,021 Views
- 41 Download
- 3 Crossref
- 0 Scopus
Abstract
Objectives
This study aimed to determine whether a mobile health (mhealth) intervention is effective in reducing weight and changing dietary behavior among employees with overweight and obesity. The study also investigated whether engagement with the intervention affected its effectiveness.
Methods
The intervention involved the use of a dietary coaching app, a wearable device for monitoring physical activity and body composition, and a messenger app for communicating with participants and an intervention manager. A total of 235 employees were recruited for a 12-week intervention from eight workplaces in Korea. Questionnaire surveys, anthropometric measurements, and 24-h dietary recalls were conducted at baseline and after the intervention.
Results
After the intervention, significant decreases in the mean body weight, body mass index, body fat percentage, and waist circumference were observed. Furthermore, the consumption frequencies of multigrain rice and legumes significantly increased, whereas those of pork belly, instant noodles, processed meat, carbonated beverages, and fast food significantly decreased compared with those at baseline. The mean dietary intake of energy and most nutrients also decreased after the intervention. When the participants were categorized into three groups according to their engagement level, significant differences in anthropometric data, dietary behaviors, and energy intake were observed following the intervention, although there were no differences at baseline, indicating that higher engagement level led to greater improvements in weight loss and dietary behavior.
Conclusions
The intervention had positive effects on weight loss and dietary behavior changes, particularly among employees with higher engagement levels. These results indicate the importance of increasing the level of engagement in the intervention to enhance its effectiveness. The mhealth intervention is a promising model for health promotion for busy workers with limited time.
- Keywords: mobile health; mobile application; dietary coaching; wearable device; engagement
Published online Apr 30, 2023.
https://doi.org/10.5720/kjcn.2023.28.2.141
Effectiveness of a mobile health intervention on weight loss and dietary behavior changes among employees with overweight and obesity: a 12-week intervention study investigating the role of engagement
-
1Doctoral student, Department of Food and Nutrition, Chungbuk National University, Cheongju, Korea.
-
2Associate professor, Department of Food and Biotechnology, Korea University, Sejong, Korea.
-
3Invited professor, Department of Food and Nutrition, Chungbuk National University, Cheongju, Korea.
-
4Master’s graduate, Department of Food and Nutrition, Chungbuk National University, Cheongju, Korea.
-
5Invited professor, Department of Food and Nutrition, Wonkwang University, Iksan, Korea.
-
6Professor, Department of Food and Nutrition, Wonkwang University, Iksan, Korea.
-
7Professor, Department of Food and Nutrition, Chungbuk National University, Cheongju, Korea.
-
1Doctoral student, Department of Food and Nutrition, Chungbuk National University, Cheongju, Korea.
- Corresponding author: Taisun Hyun. Department of Food and Nutrition, Chungbuk National University, Chungdaero-1, Heungduk-gu, Cheongju, Chungbuk 28644, Korea. Tel: +82-43-261-2790, Fax: +82-43-267-2742, Email: taisun@cbnu.ac.kr
This is an Open-Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-
Abstract
Objectives
This study aimed to determine whether a mobile health (mhealth) intervention is effective in reducing weight and changing dietary behavior among employees with overweight and obesity. The study also investigated whether engagement with the intervention affected its effectiveness.
Methods
The intervention involved the use of a dietary coaching app, a wearable device for monitoring physical activity and body composition, and a messenger app for communicating with participants and an intervention manager. A total of 235 employees were recruited for a 12-week intervention from eight workplaces in Korea. Questionnaire surveys, anthropometric measurements, and 24-h dietary recalls were conducted at baseline and after the intervention.
Results
After the intervention, significant decreases in the mean body weight, body mass index, body fat percentage, and waist circumference were observed. Furthermore, the consumption frequencies of multigrain rice and legumes significantly increased, whereas those of pork belly, instant noodles, processed meat, carbonated beverages, and fast food significantly decreased compared with those at baseline. The mean dietary intake of energy and most nutrients also decreased after the intervention. When the participants were categorized into three groups according to their engagement level, significant differences in anthropometric data, dietary behaviors, and energy intake were observed following the intervention, although there were no differences at baseline, indicating that higher engagement level led to greater improvements in weight loss and dietary behavior.
Conclusions
The intervention had positive effects on weight loss and dietary behavior changes, particularly among employees with higher engagement levels. These results indicate the importance of increasing the level of engagement in the intervention to enhance its effectiveness. The mhealth intervention is a promising model for health promotion for busy workers with limited time.
Introduction
Obesity has been identified as a major risk factor for several chronic illnesses, including cardiovascular diseases, diabetes, and some types of cancer [1]. Therefore, the prevention and management of obesity are crucial. In 2021, the prevalence of obesity with a body mass index (BMI) of 25 kg/m2 or above in Korean adults was 37.1%, with men having a higher prevalence rate (46.3%) than women (25.7%) [2]. The prevalence of obesity in women increased with age, peaking at 40.3% among those aged 60-69 years, whereas that in men was the highest in their 30s and 40s, with rates of 51.4% and 57.7%, respectively [2].
Adults in their 30s and 40s, who spend a significant amount of their time at work, tend to have unhealthy dietary habits, such as skipping breakfast, eating out frequently, eating irregularly, and binge eating, as well as health risk factors, such as drinking, smoking, and lack of exercise [3, 4, 5, 6, 7]. Furthermore, they often face challenges in maintaining their health and encounter difficulties in accessing healthcare services offered by public health centers or medical institutions owing to their busy schedule and lifestyle. A study conducted on industrial workers demonstrated that they desired regular nutrition education and counseling at their workplaces [7]. Previous studies on workplace healthcare interventions have shown positive impacts on dietary habits and health outcomes, including weight loss, of employees [8, 9, 10, 11, 12]. These results highlight the importance of implementing effective healthcare interventions in the workplace.
Recent advances in information and communication technology have led to the development of mobile healthcare, which can track and manage certain health data without the need to meet a healthcare provider using smartphones and wearable devices. Mobile health (mhealth) intervention, aimed at promoting health without any time and space limitations, is gaining momentum [13]. As of 2022, 94.2% and 21.0% of Koreans owned smartphones and wearable devices, respectively [14]. A considerable proportion (30.3%) of wearable device owners reported using them for health and fitness purposes [14]. Therefore, smartphones and wearable devices can be used as promising tools for improving the health of individuals or specific groups in certain settings, such as workplaces. Mhealth interventions have been shown to be effective in promoting health behavior changes among employees [15].
Motivation and active engagement are crucial for mhealth interventions to be effective in promoting such changes [12, 15, 16]. Engagement is defined as the extent of app usage and is an important factor in increasing the effectiveness in mhealth interventions [17]. Engagement metrics, such as login frequency, app usage time, and the number of pages visited, have been demonstrated to be positively correlated with increased physical activity and weight loss [17, 18, 19, 20, 21, 22]. However, the current literature lacks information on whether engagement levels are linked to changes in dietary behaviors or nutrient intake.
The present study aimed to evaluate the effect of a mhealth intervention on weight loss and dietary behavior changes among employees with overweight and obesity. The intervention involved the use of a dietary coaching app, a wearable device for monitoring physical activity and body composition, and a messenger app for communicating with participants and an intervention manager. The study was conducted for 12 weeks, during which we investigated the effects of the intervention on weight loss, dietary behavior changes, and nutrient intake. Our hypothesis was that the level of engagement in the intervention is related to the outcomes. Therefore, we aimed to compare the outcomes among the three groups of participants in terms of the extent of their app use.
Methods
Ethics statementThe study was approved by the Institutional Review Board of Chungbuk National University (CBNU-201906-BMSB-0113). All participants were informed of the study purposes and protocols, and they provided written informed consent. |
1. Study participants and recruitment methods
The recruitment of workplaces to implement the intervention involved explaining the purpose and content of the study to persons in charge of public institutions and small and medium-sized enterprises in Seoul, Gyeonggi, and Chungcheong. Eight workplaces from seven companies with more than 100 but less than 500 employees were recruited, and each workplace recruited more than 30 employees. The researchers provided posters, leaflets, and the applications to each business site to promote the purpose and procedure of the intervention. Interested employees were instructed to write down their height and weight on the application form and submit it to the person in charge of their workplace. Of the 293 applicants, 266 with a BMI of 23 kg/m2 or above participated in the pre-intervention survey and the 12-week intervention. The intervention was conducted from July to October 2019, and the data of a total of 235 employees were analyzed, excluding 7 who left the company, 3 who voluntarily withdrew, and 21 who did not participate in the post-intervention survey.
2. Research methods
1) Purpose of the intervention
The purpose of the 12-week healthcare intervention was to enhance the ability of employees with overweight and obesity to manage healthy eating and lifestyle using a dietary coaching app and a wearable device, to facilitate weight loss, and to improve their overall health status.
2) Mobile Apps
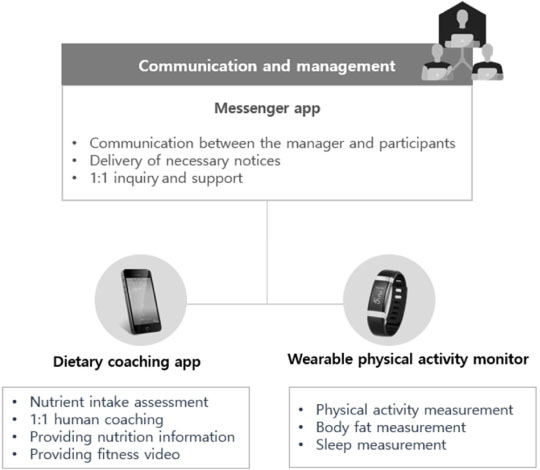
The features of the apps used in the intervention are as presented in Fig. 1.
Fig. 1
The features of the apps used in the intervention
(1) Dietary coaching app
A dietary coaching app, specifically the NOOM (Noom Korea, Korea), was purchased and provided to the participants. The NOOM offers evaluation results of nutrient intake based on the type and amount of food recorded by the participant, 1:1 coaching service, nutrition information, and step-by-step exercise and stretching videos. The participants were required to record their meals at least 2 days a week using the app to check nutrient intake and receive 1:1 coaching service.
(2) Wearable device that can monitor physical activity and body composition
A smartband, the InBody band 2 (InBody, Korea), was purchased and provided to the participants for the monitoring of their physical activity and body composition. This device is worn on the wrist and measures body composition effortlessly, providing information on the amount of activity, such as walking and exercise, in addition to percentage of body fat and muscle mass. The participants were required to wear the band daily, link it with the app once a day to check their physical activity, and measure their body composition at least once a week.
(3) Messenger app
KakaoTalk (Kakao, Korea) was used for communication and support for the participants in the intervention. The manager could simultaneously send messages to multiple people from a single account for necessary notices during the intervention. Furthermore, the participants could contact the manager at any time through 1:1 chat.
3) Pre-intervention survey
In July 2019, a pre-intervention survey was conducted in each workplace, either in a conference room or a cafeteria. The survey schedule and location were determined in consultation with the site supervisor, considering the time zone of each participant for their convenience. Before the survey, the details of the intervention were explained to the participants, and they signed a written consent form to participate in the intervention study and to provide information collected from the app to the researchers. After conducting a questionnaire survey, anthropometric measurement, and dietary assessment, the apps were installed on the participant’s smartphone.
(1) Questionnaire survey
About 1 week prior to the pre-intervention survey, an intervention description and a self-administered questionnaire were distributed to the participants to examine their general characteristics, dietary behavior and lifestyle habits. General characteristics included gender, age, marital status, educational level, average monthly income, occupation, and shift work. Dietary behavior and lifestyle habits were assessed using the Cardiovascular and Metabolic Disease Health Risk Assessment Question from the Diet-Related Health Risk Appraisal (D-HRA) [23]. The D-HRA consists of 8 questions of basic information and 15 questions of dietary behavior to assess the risk of chronic diseases through the diagnosis of individual eating habits. Basic information includes gender, age, height, weight, educational level, alcohol consumption, smoking, and activity level. Alcohol consumption is categorized as “rarely”, “once a month”, “≥twice a month”, “≥twice a week and < 7 drinks at once”, and “≥twice a week and ≥7 drinks at once”. Smoking is categorized as “does not smoke”, “< 1 pack a day”, and “≥1 pack a day"; and activity level as “inactive”, “average”, and “active”. Dietary questions include the consumption frequency of fruits, multigrain rice, milk and dairy products, legumes, fish, pork belly, instant noodles, processed meat products, carbonated beverages, and fast food, as well as the frequency of breakfast and eating out. In addition to the D-HRA questions, the frequency of eating three times a day, mealtime regularity, meal duration, amount of meals, snack frequency, and exercise frequency of at least 30 min a day were included in the final questionnaire with reference to previous studies [5, 6, 24].
(2) Anthropometric measurement
During the anthropometric measurement, the participants were instructed to remove metal items, such as rings and watches. Trained investigators measured the participants’ height, weight, body composition, and waist circumference. Height was measured to the nearest 0.1 cm using a portable extensometer, InLabS 50 (InBody, Korea). Weight and body composition were measured using InBody 570 (InBody, Korea) with open arms after the participants wiped their hands and feet with tissues. Waist circumference was measured to the nearest 0.1 cm using a smart tape measure (Bagel Labs, Korea) in the horizontal plane midway between the lowest ribs and the iliac crest while exhaling.
(3) Dietary assessment
A trained dietitian investigated the type and amount of food consumed by the participants on the preceding day by a 24-h recall method. To enhance the participants’ memory recall, they were asked to write a list of foods consumed or capture images using a mobile phone. During the survey, photos of food and dishes were presented to the participants to facilitate the amount estimation [25].
Nutrient intake was calculated using CAN-Pro 5.0 (Web ver.) of the Korean Nutrition Society [26]. The Index of Nutritional Quality (INQ) was calculated for nine nutrients, including protein, vitamin A, thiamin, riboflavin, niacin, vitamin C, calcium, phosphorus, and iron, according to the 2020 Korean Dietary Reference Intakes [27]. INQ is determined by comparing the intake of a specific nutrient per 1,000 kcal to the Recommended Nutrient Intake (RNI) of the same nutrient per 1,000 kcal, and values greater than 1 indicate a higher nutrient density than energy consumed.
(4) App installation
Once the pre-intervention survey was finished, the participants were given smartbands and were assisted in installing the dietary coaching app, smartband app, and messenger app on their smartphones. The investigators also provided instructions regarding the use of each app during the 12-week period and handed out checklists for participants to track their daily progress. Any inquiries during the intervention could be directed to the investigators through the messenger app at any time.
4) Intervention process and management
The manager of the intervention collected app-generated data on a weekly basis throughout the intervention period. A password file was sent via email from the company to the manager. The manager devised strategies to boost engagement and promote behavioral changes based on the participants’ engagement levels. In the first 3 weeks, content was shared via KakaoTalk to help participants adapt to the intervention. At week 4, mobile coupons were offered as incentives for exceptional participants. Participants with an engagement of less than 50% received encouraging messages at week 5, and phone calls were made if necessary. At week 6, the participants were informed of changes in body fat, and at week 7, engagement level by workplace was announced. Weeks 8-11 consisted of reinforcement of engagement by weekly events with rewards. At week 12, outstanding participants and companies were promised a reward plan following the intervention.
5) Post-intervention survey
Post-intervention survey was conducted at the workplace using the same methodology as the pre-intervention survey. After anthropometric measurements, the participants were informed of their changes in weight and body composition during the 12-week intervention. Individual nutrition counseling was also provided, and the participants were given nutrition information to continue managing their health even after the intervention ended.
6) Categorization of engagement level
Engagement level was calculated by scoring the information obtained from the participant’s app usage data. To ensure equal weighting of the dietary coaching and smartband usage, the scores obtained from each were converted to a maximum of 50 points and then combined for a total out of 100. To achieve a score for the dietary coaching app usage, meal records for at least 2 days a week were required, with 1 point awarded per week for meeting this threshold and a maximum score of 12 points, which was then converted to 50 points. For the smartband usage, a score was awarded for wearing the device every day and linking it to the app, with a maximum score of 84 points. In addition, a score was awarded for measuring body fat at least once a week, with 1 point per week and a maximum score of 12 points. The two smartband usage scores were given equal weight, with a maximum of 25 points each, making the overall score 50 points.
To improve interpretability, the participants were categorized into three groups based on fixed score ranges of engagement levels: (1) those with a score of 80 points or higher (upper group, UPG), (2) those with a score of lower than 80 points but 50 points or higher (median group, MDG), and (3) those with a score of lower than 50 points (lower group, LG).
3. Statistical analysis
The categorical variables were expressed as frequency and percentage, and the continuous variables as mean and standard deviation. To compare pre- and post-intervention data, the McNemar test and paired t-test were used for categorical and continuous variables, respectively. To determine the differences in anthropometric data, dietary behavior, lifestyle habits, and nutrient intake among the UPG, MDG, and LG before and after the intervention, categorical variables were analyzed using the χ2-test, whereas continuous variables were analyzed using analysis of variance, followed by Duncan’s multiple range test. After the intervention, the differences among the UPG, MDG, and LG were also analyzed using analysis of covariance corrected for pre-intervention results for continuous variables. Data analysis was conducted using SAS version 9.4 (SAS Institute Inc. Cary, NC, USA), and the significance level for all analyses was set at P < 0.05.
Results
1. General characteristics
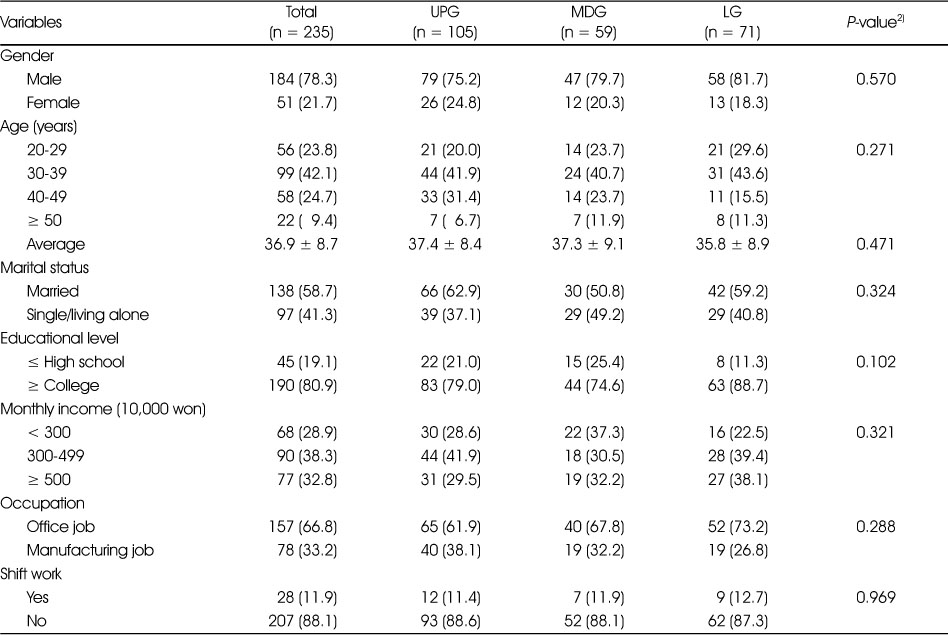
Table 1 presents the general characteristics of the participants. The majority (78.3%) of the participants were men, with 42.1% being in their 30s and 24.7% in their 40s. The average age of the participants was 36.9 years. Furthermore, 58.7% of the participants were married, and 80.9% had a college degree or higher. Approximately 38.3% of the participants had a monthly income of between 3 and 4.99 million won, and 32.8% had an income of at least 5 million won. Regarding occupation, 66.8% of the participants were office workers, 33.2% were production workers, and 11.9% worked shifts. No significant differences were observed in the general characteristics of the participants across the three different engagement groups.
Table 1
General characteristics of the participants according to engagement level1)
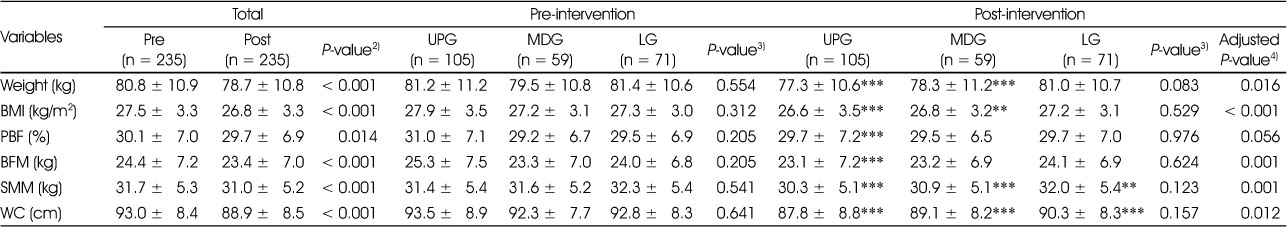
2. Anthropometric changes pre- and post-intervention
Table 2 demonstrates significant reductions in weight (P < 0.001), BMI (P < 0.001), percentage of body fat (P < 0.05), body fat mass (P < 0.001), skeletal muscle mass (P < 0.001), and waist circumference (P < 0.001) after the intervention. When the participants were categorized into three groups according to their engagement level, the UPG showed significant reductions in all six indicators after the intervention (P < 0.001). The MDG showed significant reductions in weight (P < 0.001), BMI (P < 0.01), skeletal muscle mass (P < 0.001), and waist circumference (P < 0.001) but not in body fat mass or percentage of body fat. The LG only showed significant reductions in skeletal muscle mass (P < 0.01) and waist circumference (P < 0.001).
Table 2
Anthropometric changes pre- and post-intervention, stratified by engagement level1)
No significant differences in anthropometric variables were observed between the UPG, MDG, and LG pre- and post-intervention. However, after adjusting for pre-intervention anthropometric data, differences were observed between the three groups in weight (P < 0.05), BMI (P < 0.001), body fat mass (P < 0.01), skeletal muscle mass (P < 0.01), and waist circumference (P < 0.05). Specifically, the UPG showed a greater decrease in weight, BMI, body fat mass, skeletal muscle mass, and waist circumference than the LG after the intervention.
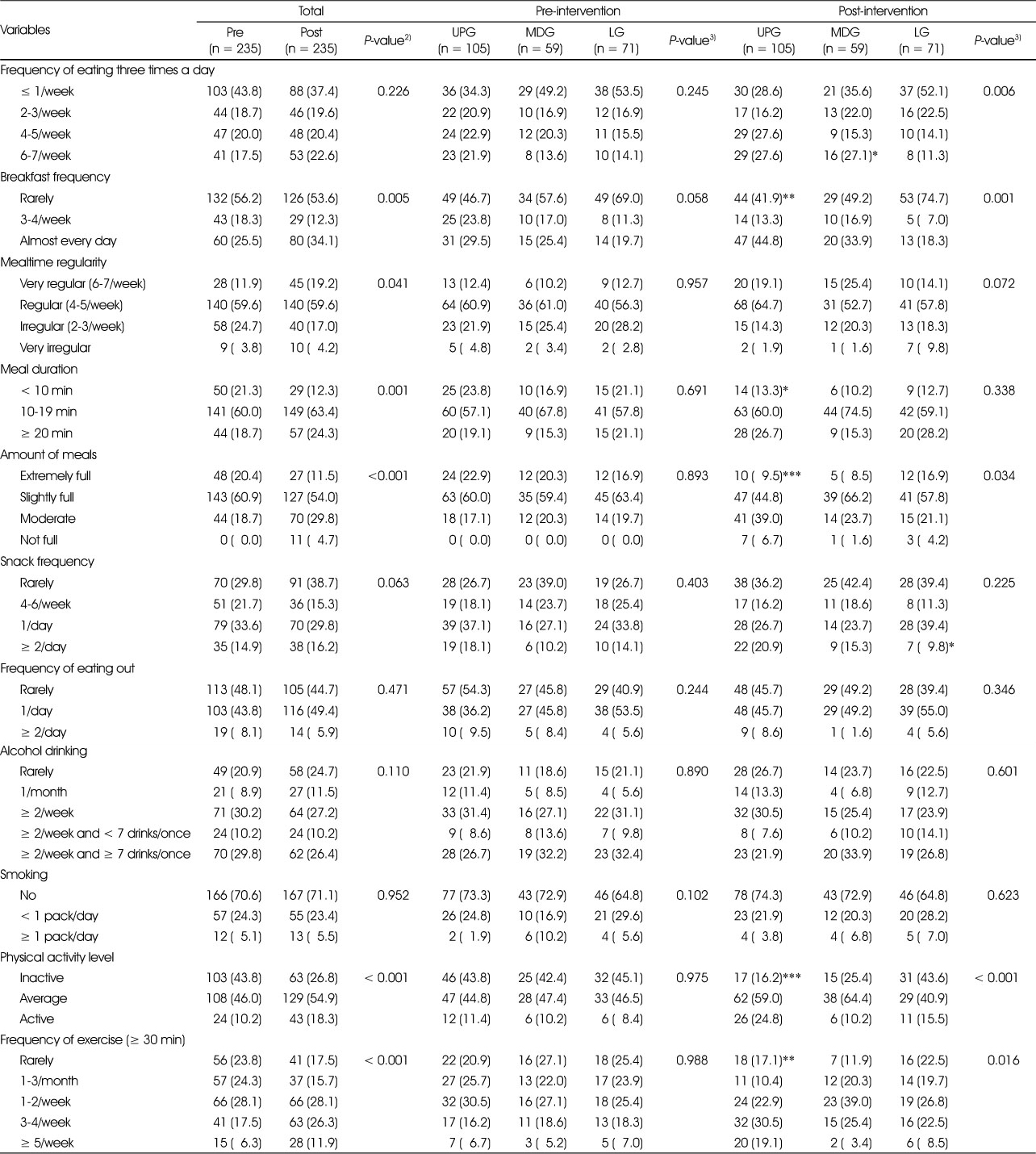
3. Dietary and lifestyle habit changes pre- and post-intervention
The dietary and lifestyle habit changes pre- and post-intervention are presented in Table 3. After the intervention, significant changes in breakfast frequency (P < 0.01), mealtime regularity (P < 0.05), meal duration (P < 0.01), amount of meals (P < 0.001), physical activity level (P < 0.001), and frequency of exercise for at least 30 min (P < 0.001) were observed. Specifically, breakfast frequency increased from 25.5% to 34.1% for “almost every day”, and mealtime regularity increased from 11.9% to 19.2% for “very regular”. Meal duration “less than 10 min” decreased from 21.3% to 12.3% , and the rate of eating “extremely full” and “slightly full” decreased from 81.3% to 65.5%. The percentage of physical activity being “active” and exercising “≥3/week” for at least 30 min increased from 10.2% to 18.3% and from 23.8% to 38.2%, respectively.
Table 3
Dietary and lifestyle habit changes pre- and post-intervention, stratified by engagement level1)
When comparing pre- and post-intervention in the UPG, there were significant differences in breakfast frequency (P < 0.01), meal duration (P < 0.05), amount of meals (P < 0.001), physical activity level (P < 0.001), and frequency of exercise for at least 30 min (P < 0.01). In the MDG, there was a significant difference in the frequency of eating three times a day (P < 0.05), and in the LG, there was a significant difference in snack frequency (P < 0. 05).
Prior to the intervention, no significant differences were observed between the UPG, MDG, and LG in all categories of dietary and lifestyle habits. However, significant differences were observed between the three groups in the frequency of eating three times a day (P < 0.01), breakfast frequency (P < 0.01), amount of meals (P < 0.05), physical activity level (P < 0.001), and frequency of exercise for at least 30 min (P < 0.05) after the intervention. In terms of the frequency of eating three times a day, the UPG and MDG had a higher frequency of eating “6-7 days/week” (27.6% and 27.1%, respectively) compared with the LG (11.3%). The UPG also had a higher proportion of eating “almost every day” for breakfast (44.8%) compared with the MDG (33.9%) and LG (18.3%). Furthermore, the UPG had a higher proportion of eating “moderately” (39.0%) compared with the MDG (23.7%) and LG (21.1%). In terms of physical activity level, the UPG had a higher proportion of “active” (24.8%) compared with the MDG (10.2%) and LG (15.5%). Finally, the proportion of participants exercising “≥3/week” for at least 30 min was higher in the UPG (49.6%) than in the MDG (28.8%) and LG (31.0%).
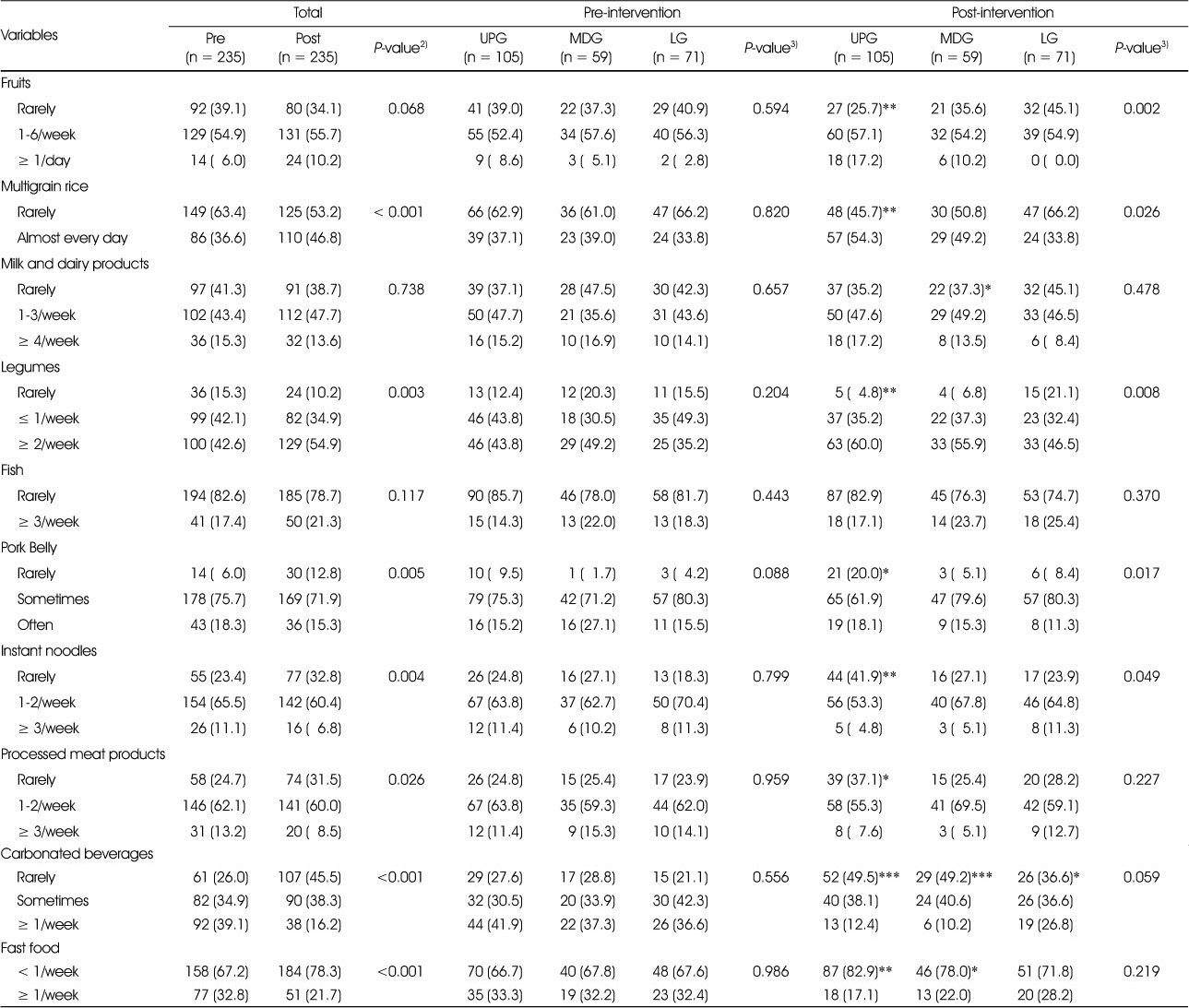
4. Changes in food group consumption frequencies pre- and post-intervention
Table 4 presents the changes in food group consumption frequencies pre- and post-intervention. After the intervention, the consumption frequencies of multigrain rice (P < 0.001) and legumes (P < 0.01) significantly increased, whereas those of pork belly (P < 0.01), instant noodles (P < 0.01), processed meat (P < 0.05), carbonated beverages (P < 0.001), and fast food (P < 0.001) significantly decreased. Specifically, the proportion of participants who reported eating multigrain rice “almost every day” and legumes “twice a week or more” significantly increased from 36.6% to 46.8% and from 42.6% to 54.9%, respectively. Conversely, the proportion of participants who reported eating pork belly “rarely” increased from 6.0% to 12.8%. In addition, the proportion of participants who reported “rarely” eating instant noodles and processed meat increased from 23.4% to 32.8% and from 24.7% to 31.5%, respectively. Furthermore, the proportion of participants who reported “rarely” drinking carbonated beverages significantly increased from 26.0% to 45.5%, and the proportion of participants who reported eating fast food “less than once a week” significantly increased from 67.2% to 78.3%.
Table 4
Changes in food group consumption frequencies pre- and post-intervention, stratified by engagement level1)
After the intervention, the UPG showed significant improvement in the consumption frequencies of all food groups, except for milk and dairy products, and fish, whereas the MDG showed an increase in the consumption frequency of milk and dairy products (P < 0.05) and a decrease in the consumption frequencies of carbonated beverages (P < 0.001) and fast food (P < 0.05). Contrarily, the LG only showed significant decrease in the consumption frequency of carbonated beverages (P < 0.05).
No differences were observed in the consumption frequency of the food group among the three groups before the intervention; however, af ter the intervention, significant differences were observed in the consumption frequencies of fruit (P < 0.01), multigrain rice (P < 0.05), legumes (P < 0.01), pork belly (P < 0.05), and instant noodles (P < 0.05). The proportion of the UPG who ate fruit “at least once a day” was higher at 17.2% compared with those of the MDG at 10.2% and the LG at 0.0%. The proportion of the UPG who ate multigrain rice “almost every day” was 54.3%, whereas those of the MDG and LG were 49.2% and 33.8%, respectively. For legumes, the proportion of the UPG who ate “twice a week or more” was the highest at 60.0%, followed by the MDG at 55.9% and LG at 46.5%. The proportion of the UPG who ate pork belly “rarely” was 20.0%, whereas those of the MDG and LG were 5.1% and 8.4%, respectively. Even for instant noodles, the proportion of the UPG who ate “rarely” was the highest at 41.9%, followed by the MDG at 27.1% and LG at 23.9%.
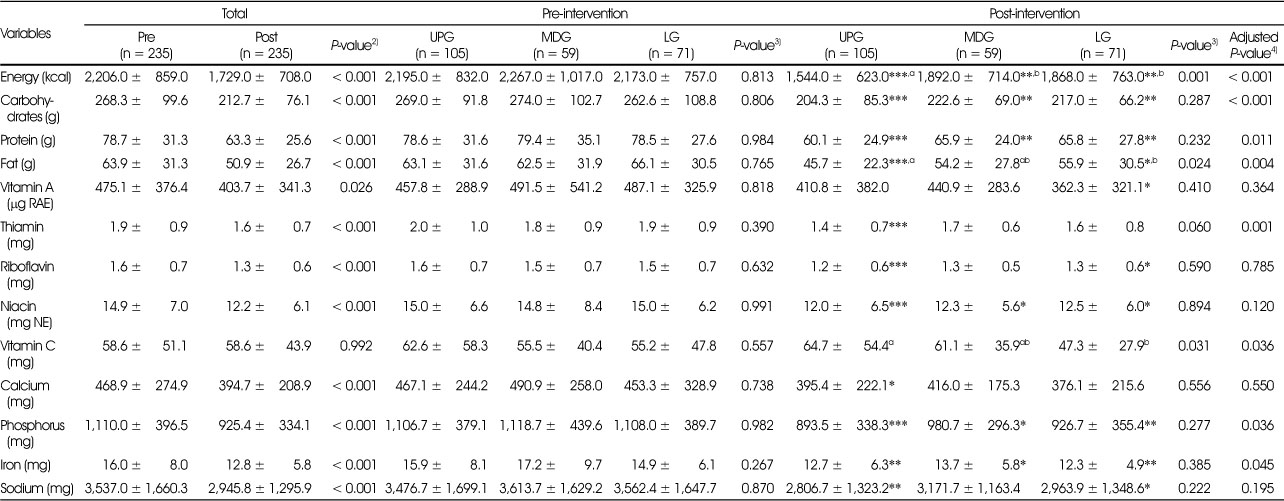
5. Changes in nutrient intake and INQ pre- and post-intervention
The changes in the average daily intake of energy and nutrients pre- and post-intervention are presented in Table 5. After the intervention, there was a significant decrease in energy (P < 0.001) and all nutrient intake (P < 0.05), except vitamin C. When comparing pre- and post-intervention in the UPG, a significant decrease in energy and all nutrient intake, except vitamin A and vitamin C was observed. In addition, intakes of energy, carbohydrates, protein, niacin, phosphorus, and iron were significantly decreased in the MDG, and intakes of energy, carbohydrates, protein, fat, vitamin A, riboflavin, niacin, phosphorus, iron, and sodium were significantly decreased in the LG.
Table 5
Changes in dietary intake of energy and nutrients pre- and post-intervention, stratified by engagement level1)
Before the intervention, no differences were observed in energy and nutrient intake among the three groups; however, after the intervention, significant differences were observed in energy (P < 0.01), fat (P < 0.05), and vitamin C (P < 0.05) intakes. The UPG had lower average daily energy intake of 1,544 kcal/day than the MDG and LG, which had 1,892 and 1,868 kcal/day, respectively. Fat intake was also lower in the UPG with 45.7 g/day than in the LG with 55.9 g/day. However, vitamin C intake was higher in the UPG with 64.7 mg/day than in the LG with 47.3 mg/day. After adjusting for baseline intake, significant differences were observed in the intakes of energy (P < 0.001), carbohydrates (P < 0.001), protein (P < 0.05), fat (P < 0.01 ), thiamin (P < 0.01), vitamin C (P < 0.05), phosphorus (P < 0.05), and iron (P < 0.05) among the three groups.
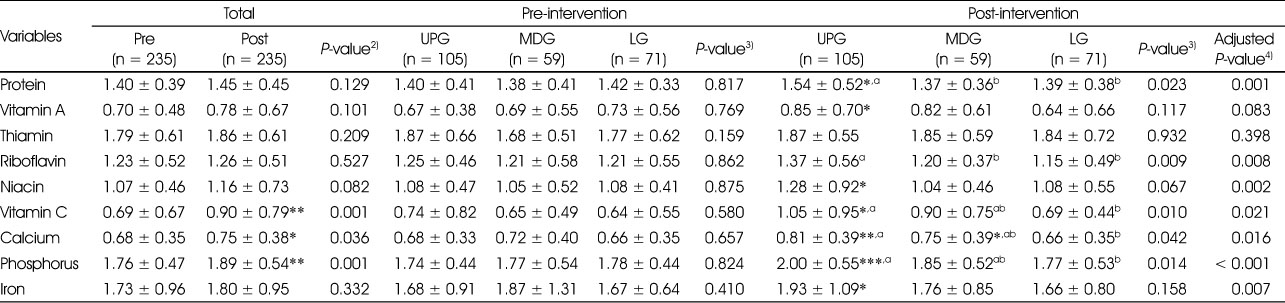
Table 6 presents the changes in INQ pre- and post-intervention. In the overall participants, the INQ of vitamin C (P < 0.01 ), calcium (P < 0.05), and phosphorus (P < 0.01) significantly increased after the intervention. When compared pre- and post-intervention in the UPG, there was a significant increase in the INQ of protein, vitamin A, niacin, vitamin C, calcium, phosphorus, and iron. In the MDG, the INQ of calcium significantly increased, whereas there were no differences in the INQ of any nutrients in the LG. Before the intervention, there were no differences in the INQ among the three groups; however, after adjusting for baseline INQ, significant differences were observed in the intake of all nutrients, except for vitamin A and thiamin, with the UPG having higher INQ than the LG.
Table 6
Changes in INQ pre- and post-intervention, stratified by engagement level1)
Discussion
The participants in the 12-week intervention, who were overweight and had obesity, achieved weight loss and had improved dietary behavior and nutrient intake. It was made possible by the use of a mobile dietary coaching app, a smartband for measuring physical activity and body composition, and a messenger app. Our findings are consistent with those of Toro-Ramos et al. [28]. They demonstrated an average weight loss of 7.5% in 104 adults with a BMI of 23 kg/m2 or higher who used a dietary coaching app for 15 weeks, and weight loss was sustained even 1 year later. Another study also obtained comparable results, which reported that 77.9% of the 35,921 users achieved weight loss when they used the app for a median of 267 days [29], indicating that the use of mobile dietary coaching apps are effective in reducing weight.
Contrarily, Cadmus-Bertram et al. reported no weight change among women with a BMI of 25 kg/m2 or higher who used a wearable device for 16 weeks [30]. In a 12-week intervention that involved the use of a smartband among patients diagnosed with metabolic syndrome, no changes in weight, body fat percentage, and waist circumference were also observed [31]. Similarly, in a study conducted on sedentary office workers using a smartband for 12 weeks, there was a significant increase in physical activity, but weight change was not reported [32]. In a meta-analysis of studies using wearable devices without dietary coaching, wearable devices were found to increase physical activity but had no effect on weight, BMI, and waist circumference reduction [33]. This suggests that dietary behavior changes must be accompanied by increased physical activity for weight loss.
The present study examined the effect of the intervention on weight loss and dietary behavior changes among the three groups with varying levels of engagement to ascertain if the group with higher engagement level yielded superior outcomes. The findings indicated that the UPG demonstrated greater improvements in weight loss and dietary behavior than the LG. No notable disparities were observed among the three groups prior to the intervention; however, significant differences were observed post-intervention, highlighting the importance of adopting strategies to enhance intervention adherence.
The UPG showed improvements in physical activity level and the frequency of exercise, in addition to dietary behavior, including the frequency of eating three times a day, breakfast frequency, and amount of meals. Active engagement seemed to have helped reducing weight by checking their dietary habits through meal records and regularly monitoring changes in their physical activity using the wearable devices. Carey et al. [21] also reported that weight loss was associated with the number of articles read, meals and exercise logged, steps recorded, messages to coach in a mhealth intervention.
Our study demonstrated that the UPG had notably healthier dietary patterns than the MDG or LG after the intervention. This was evidenced by the UPG having a higher frequency of consuming fruits, multigrain rice, and legumes and lower frequency of consuming pork belly and instant noodles. Previous research demonstrated that increasing whole grain intake by 30 g/day decreased the risk of being overweight and obesity by 7%, whereas increasing legume intake by 50 g/day reduced the risk by 12% [34]. These results indicate that the dietary choices made by the UPG were more favorable. Furthermore, after the intervention, the participants consumed less energy, carbohydrates, protein, fat, vitamins, and minerals on average. Notably, the UPG consumed significantly less energy and fat than the MDG or LG. Despite the decrease in energy intake, the UPG had a higher INQ for protein, riboflavin, niacin, vitamin C, calcium, phosphorus, and iron than the LG, suggesting that the UPG consumed high-density meals. It is noteworthy that only the UPG had an INQ higher than 1 for vitamin C. Although the intervention increased the INQ for calcium, an INQ of 0.75 was still insufficient. Recent data from the 2021 Korea National Health and Nutrition Examination Survey indicated that adults aged 19 years and above consumed only 64.3% of the RNI, making it one of the most deficient nutrients [2]. Studies have suggested that calcium-rich dairy products can help reduce body weight and fat mass as well as preventing cardiovascular disease and diabetes [35]. Thus, education to increase calcium intake is necessary.
The challenge that participants faced during the intervention was that the body composition data was not integrated with the dietary coaching app, requiring the use of two separate apps. The manager continued to motivate participants and address any issues they encountered while using the apps through messages. While this study had a limitation in that it compared pre- and post-intervention results of a single group without a control group, it was observed that a higher engagement level was more effective in reducing weight and changing dietary behavior. Thus, this limitation may be mitigated. Previous studies often used self-reported weights, which may have limitations [21]; however, our study had the advantage of actually measuring weight and body composition using highly validated devices. Furthermore, this intervention had a high retention rate (88.3%), indicating that the participants were committed to completing the full 12-week intervention. This study emphasized the importance of engagement in improving dietary behavior and nutrient intake, and achieving weight loss. Future studies should explore effective strategies for increasing engagement in mhealth intervention.
Conclusion
The mhealth intervention used in this study was effective in promoting weight loss and improving dietary behavior among employees with overweight and obesity, particularly those with a high level of engagement. This intervention is expected to be a good model for busy workers with limited time for healthcare.
Conflict of Interest:There are no financial or other issues that might lead to conflict of interest.
Funding:This study was supported by Korea Health Industry Development Institute.
Data availability
The participants of this study did not give written consent for their data to be shared publicly, so due to the sensitive nature of the research supporting data is not available.
References
-
World Health Organization (WHO). Obesity and overweight [internet]. World Health Organization; 2021 [cited 2023 Mar 31].Available from: https://www.who.int/news-
room/fact- sheets/detail/obesity- and- overweight .
-
-
Korea Disease Control and Prevention Agency. Korea Health Statistics 2021: Korea National Health and Nutrition Examination Survey (KNHANES VIII-3) [internet]. Korea Disease Control and Prevention Agency; 2022 [cited 2022 Dec 30].Available from: https://knhanes.kdca.go.kr .
-
-
Cho SH, Jang JH, Ha TY, Lee KS, Kim MK, Seo JS. A survey on breakfast of workers in Daegu area. Korean J Community Nutr 2004;9(6):673–682.
-
-
Lee MA, Lee EJ, Soh HK, Choi BS. Analysis on stress and dietary attitudes of male employees. Korean J Community Nutr 2011;16(3):337–352.
-
-
Hong YH, Lee EH, Lim HS, Chyun JH. Dietary habits and the perception and intake of health functional foods in male office workers by age. J East Asian Soc Dietary Life 2015;25(2):340–351.
-
-
Park SH, Lee EJ, Chang KJ. Dietary habits and snack consumption behaviors according to level of job stress among 20-to 30-year old office workers in the Seoul metropolitan area. J Korean Soc Food Cult 2020;35(2):143–155.
-
-
Yim JS, Heo YR. A qualitative study of the awareness and influencing factors of the dietary habits of the male and female workers' at a manufacturing facility in Gwangju. Korean J Community Nutr 2022;27(1):12–26.
-
-
Park SY, Yang YJ, Kim Y. Effects of nutrition education using a ubiquitous healthcare (u-health) service on metabolic syndrome in male workers. Korean J Nutr 2011;44(3):231–242.
-
-
Han SR, Yu OK, Byun MS, Park TS, Cha YS. Effects of a weight management program for overweighted or obese office workers. J Korean Soc Food Sci Nutr 2013;42(10):1608–1617.
-
-
Kim HJ, Choi I, Kim WG, Asano K, Hong J, Cho YM, et al. Effect of a worksite-based dietary intervention program for the management of metabolic syndrome. Korean J Community Nutr 2016;21(3):237–246.
-
-
Sandercock V, Andrade J. Evaluation of worksite wellness nutrition and physical activity programs and their subsequent impact on participants' body composition. J Obes 2018:1035871
-
-
Korea Information Society Development Institute. 2022 Korea Media Panel Survey [internet]. Korea Information Society Development Institute; 2022 [cited 2023 Mar 31].Available from: https://www.kisdi.re.kr/report/view.do?key=m2101113024973&arrMasterId=3934581&masterId=3934581&artId=1131416 .
-
-
Buckingham SA, Williams AJ, Morrissey K, Price L, Harrison J. Mobile health interventions to promote physical activity and reduce sedentary behaviour in the workplace: A systematic review. Digit Health 2019;5:2055207619839883
-
-
Valinskas S, Nakrys M, Aleknavičius K, Jonusas J, Lileikienė A. User engagement and weight loss facilitated by a mobile app: Retrospective review of medical records. JMIR Form Res 2023;7(1):e42266
-
-
Korea Health Industry Development Institute. Diet related Health Risk Appraisal (D-HRA) [internet]. Korea Health Industry Development Institute; 2016 [cited 2023 Mar 31].Available from: https://khidi.or.kr/dhra .
-
-
Cho S, Kim J, Jo YM, Han YH, Yeoh Y, Yon MY, et al. Impact of personalized goal setting and smartphone-based nutrition counseling on dietary habit improvement and weight loss among city bus drivers with overweight and obesity. J Hum Ecol 2022;26(2):81–98.
-
-
Korea Disease Control and Prevention Agency, National Institute of Health. Photos for quantity estimation: Korean Genome and Epidemiology Study. Cheongju: Korea Disease Control and Prevention Agency; 2015.
-
-
The Korean Nutrition Society. CAN-Pro 5.0 (Web ver.) Professional [Internet]. The Korean Nutrition Society; 2015 [cited 2023 Mar 31].Available from: https://www.kns.or.kr/can/CanPro5.asp .
-
-
Ministry of Health and Welfare, The Korean Nutrition Society. Revision of 2020 Dietary Reference Intakes for Koreans. Sejong: Ministry of Health and Welfare; 2020.
-
-
Chin SO, Keum C, Woo J, Park J, Choi HJ, Woo JT, et al. Successful weight reduction and maintenance by using a smartphone application in those with overweight and obesity. Sci Rep 2016;6(1):34563
-
-
Ha Y. Effectiveness of a mobile wellness program to increase physical activity in office workers. J Digit Converg 2019;17(11):369–376.
-
Figure & Data
References
Citations

- Improving the nutrition quotient and dietary self-efficacy through personalized goal setting and smartphone-based nutrition counseling among adults in their 20s and 30s
Dahyeon Kim, Dawon Park, Young-Hee Han, Taisun Hyun
Journal of Nutrition and Health.2023; 56(4): 419. CrossRef - Process evaluation of a mobile healthcare program among employees with overweight and obesity: a 12-week intervention study investigating the role of engagement
Imhuei Son, Jiyoun Hong, Young Hee Han, Bo Jeong Gong, Meng Yuan Zhang, Woori Na, Cheongmin Sohn, Taisun Hyun
Korean Journal of Community Nutrition.2023; 28(6): 466. CrossRef - Systematic Review on the Study of the Childhood and Adolescent Obesity in Korea: Dietary Risk Factors
Eun Jeong Heo, Jae Eun Shim, Eun Young Yoon
Korean Journal of Community Nutrition.2017; 22(3): 191. CrossRef

 KSCN
KSCN
 Cite
Cite


